When a thigh cramp or leg pain occurs during sleep, it can happen suddenly and painfully — which isn’t unusual with diabetes, neuropathy, and obesity. Muscle cramps can affect any part of your leg, though calf and thigh cramps are the most common.
However, other issues can also contribute to the pain and suffering.
Your Thigh Cramp and the World of Nocturnal Pain
Many adults across the United States report having ongoing nocturnal leg cramps, and especially a thigh cramp, according to studies. It causes severe insomnia and is usually impacted by recurrent, painful tightening in the calf muscles. While a precise reason is unknown, it’s likely muscle fatigue, nerve dysfunction, and blood vessel impairment cause your back of leg cramps at night — not necessarily electrolyte imbalance.
The causes of nocturnal leg cramps include vascular disease, spinal canal stenosis, cirrhosis, hemodialysis, pregnancy, and other conditions. Doctors and institutions associate some medications with leg cramps. This list includes intravenous iron sucrose, conjugated estrogens, raloxifene, naproxen, and teriparatide. In addition, you can differentiate restless legs syndrome, claudication, myositis, and peripheral neuropathy from nocturnal leg cramps with a history of physical examination.
Back of thigh cramps at night are difficult to treat, as well as leg cramps (also known as “charlie horses”). There is uncertainty about the etiology, appropriate diagnostic evaluation, and the best treatment. There are many children and adults who experience nocturnal leg cramps. The prevalence of these conditions increases with age, and they are slightly more common in women. The symptoms of leg cramps are bothersome enough to prompt patients to seek medical attention 20 percent of the time.
The Symptoms
An average leg cramp lasts nine minutes and is painful and incapacitating. Recurrences and residual pain may follow the acute episode for hours. Secondary insomnia is typically associated with leg cramps that occur at night. It is most common to experience cramps in the posterior calf muscles, but thigh or foot cramps are also common. There are several types of leg cramps, including spasms, tightening, twinges, strains, tetany, swellings, or seizures. It is possible for cramps to be isometric or to cause limb movements, for example, extreme plantar flexion of the foot.
In spite of this, leg cramps offer family physicians an opportunity to diagnose and treat conditions such as venous insufficiency, peripheral vascular disease, and peripheral neuropathy. The difference between restless legs syndrome, leg cramps, and your thigh cramp can be difficult to distinguish, which is why the best treatment for leg cramps at night starts with a simple appointment with a pain management specialist.
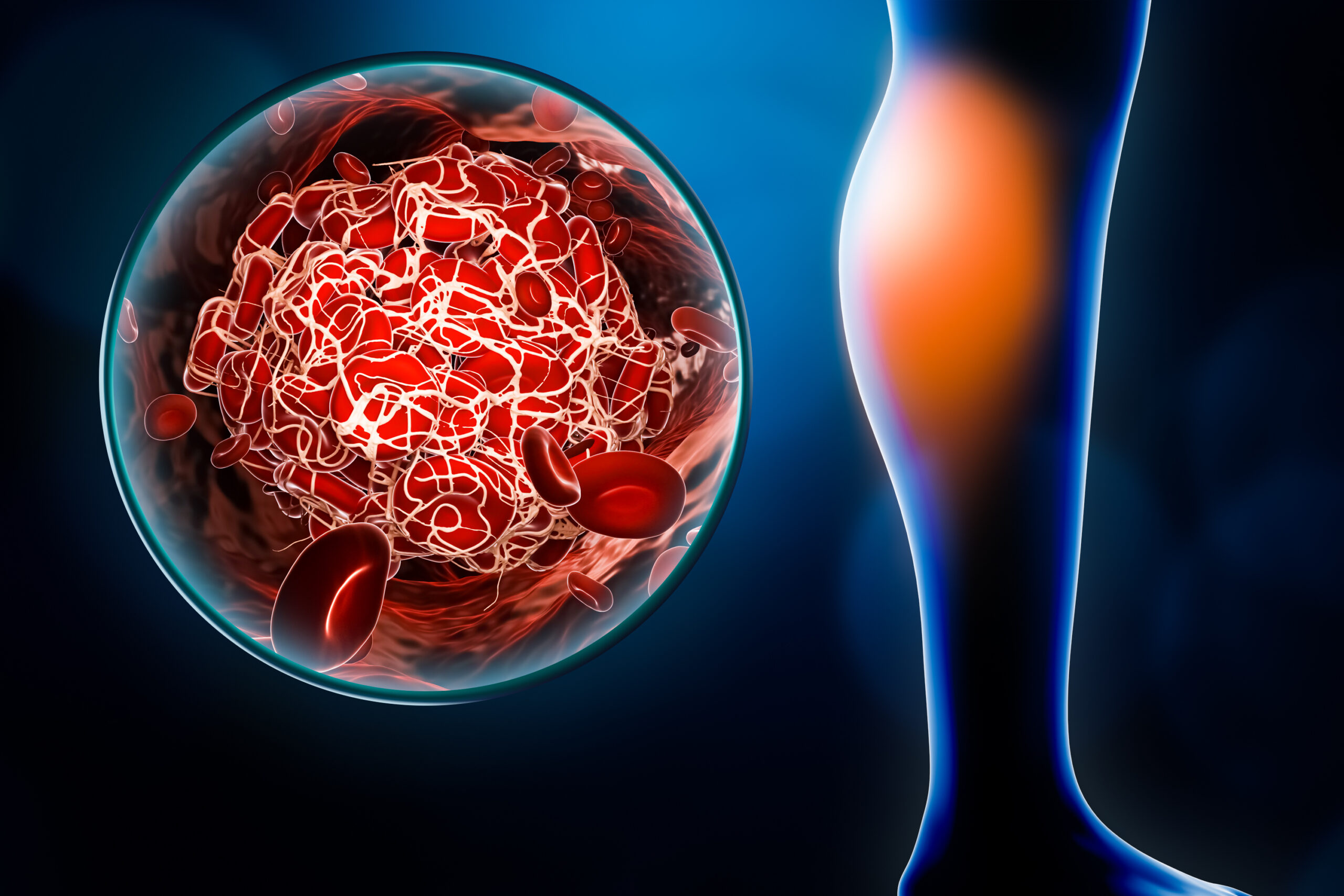
The Science Behind Venous Insufficiency and Cramping
Blood returns to the heart through deep and superficial veins in your lower extremities, which is key to understanding the bodily science surrounding your thigh cramp. Several valves within the veins are responsible for maintaining normal venous flow patterns.
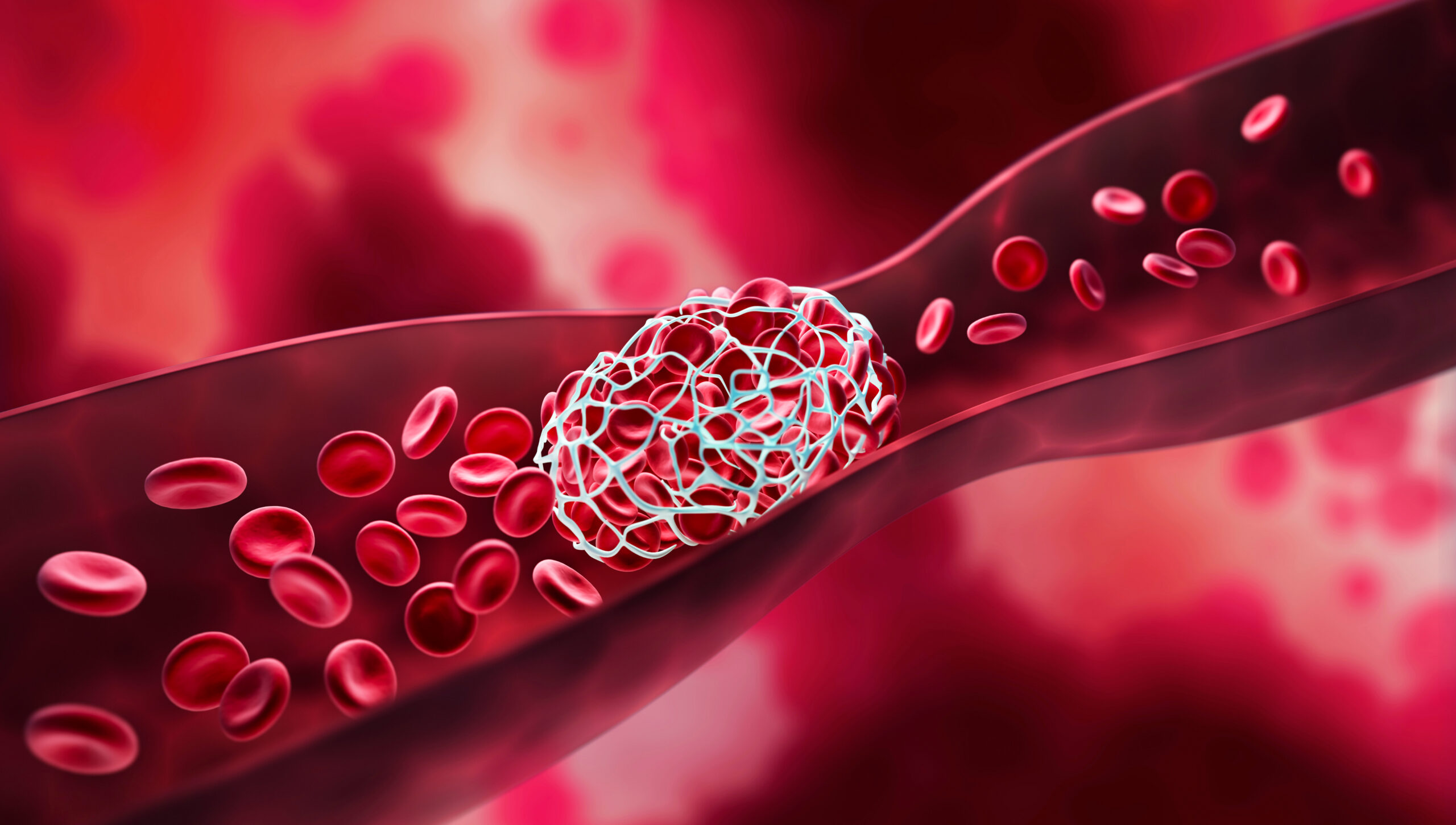
An obstruction in a vein (such as chronic thrombosis) or an incompetent valve can cause venous insufficiency. The valves in your body help blood flow in the right direction (towards your heart). It becomes impossible for a valve to close properly if it becomes damaged. Flowing upward toward the heart becomes difficult as gravity takes over. As a result, it flows backward, a condition known as venous reflux.
It’s possible to develop varicose veins when the venous valves in superficial veins become incompetent. Pain, swelling, skin changes and eventual tissue breakdown may result from chronic venous insufficiency in the deep or superficial venous system. Your back of leg cramps at night can become a common occurrence each time you lay down to sleep.
Pain management specialists can detect obstructions in the deep and superficial veins through special scanning. Specialists can also use ultrasound to determine the direction of blood flow in each segment of the evaluated veins. Often, they perform the evaluation while you’re upright. This tests the function of each valve as well.
It’s usually not necessary to evaluate the function of the lower extremity veins. However, it’s important to obtain a complete lower-extremity venous duplex scan when considering surgical treatment, sclerotherapy, or saphenous venous ablation. Both lower extremities may be included during a comprehensive check-up to explore why you’re suffering from bad calf cramps at night.
Contributing Factors: Valve Damage and Your Thigh Cramp
Valves in your leg veins can be damaged for many reasons, including blood clots, varicose veins, pregnancy, injury, and various medical conditions — bringing on a severe thigh cramp as you sleep.
Deep vein thrombosis (DVT) causes damage to the vein’s valves when blood clots form. Varicose veins also don’t help, as you may develop venous insufficiency due to these twisted, enlarged veins. Even a leg injury can damage your vein’s valves.
What’s more concerning: A pregnant woman’s veins may suffer damage due to the extra pressure during pregnancy. Her bad leg cramps at night during pregnancy are usually directly attributable to the extra weight and pressure.
Congestive heart failure could also be a common factor in your back of leg cramps at night. It happens when the heart does not pump enough blood to meet the body’s needs. Fluid can build up in the tissues, including the legs and feet, causing edema. Venous insufficiency can be caused by congestive heart failure in two ways: Increased pressure in the veins and reduced blood flow to the legs. Most patients are also suffering from venous insufficiency.
Other Medical Conditions
High blood pressure caused by chronic kidney disease can also damage your veins’ valves, causing chronic kidney disease. Blood becomes anemic when it lacks enough red blood cells to carry oxygen to tissues. Changes in blood chemistry can also cause chronic kidney disease, causing veins to become more vulnerable.
Your life can also get super complicated when you have diabetes. In addition to damaging blood vessels, high blood sugar can also damage veins. Veins can become weaker and have a harder time pumping blood back to the heart as a result. As a result of diabetes, you can also develop neuropathy, which damages your nerves and affects your control of leg muscles, causing them to weaken as a result. Peripheral artery disease, which results in the narrowing or blocking of arteries, is also associated with diabetes.
Obesity can also complicate diabetes. When you’re obese, the extra weight exerts pressure on your leg’s veins. This makes it more difficult for the heart to circulate blood fully. All these problems have directed many patients to find the best treatment for leg cramps at night.
Understanding the Internal Anatomy of Your Thigh
There are four main blood vessels in your thigh that you should consider when suffering from a thigh cramp: the femoral artery, femoral vein, popliteal artery, and popliteal vein. Thigh and lower leg blood flow is supplied by the femoral artery. Upon entering the thigh, it exits behind the knee at the popliteal fossa.
Located along the femoral artery, the femoral vein drains blood from the thigh and lower leg into the abdomen via the inguinal ligament. In addition, the popliteal artery provides blood to the knee joint and lower leg. Behind the knee, it enters the popliteal fossa and exits at the calf.
We can’t forget the popliteal vein. Blood is drained from the knee joint and lower leg through this continuation of the femoral vein. Located at the head of the popliteal artery, it terminates at the calf where it enters the popliteal fossa.
Smaller blood vessels in the thigh also supply muscles and other tissues with blood. Combined, all these vessels supply blood and nutrients to muscles and tissue as well as remove waste products. Your back of leg cramps at night are all connected to this highly complex and unique area of the body.
Thigh Cramp Symptoms, Questions, and Best Treatment
As you endure your thigh cramp nearly every night in bed, you may feel dull aching, heaviness, or cramping in both your thighs and legs. Too much time spent on your legs will cause them to swell up. You may experience itching or tingling in your legs. If you stand, your pain will be worse, and if you raise your legs, it will be better.
Symptoms stemming from back of leg cramps at night are no fun. Looking past your thighs, there may be redness in your legs and ankles. Around your ankles, you may notice changes in the color of your skin. Varicose veins may be visible on the surface of your legs. Skin on your legs and ankles may thicken and harden.
Some Options
How can you treat venous insufficiency? Compression stockings will help you reduce swelling in your legs, according to your pain management specialist. Sitting or standing for long periods of time is probably not a good idea. The blood in your veins will return to your heart even if you move your legs slightly.
In the same way, walking helps. Varicose veins may require surgery or other treatments if you have tried everything and still have leg pain, skin ulcers, or sores caused by poor blood flow. Anticoagulant or blood-thinning medicines may be prescribed by your doctor if blood clots are causing you problems.
When lying down, your pain management specialist may also suggest elevating your legs above your heart. Exercise can also improve your circulation, and swelling and venous insufficiency can be treated with weight loss as well.
Insufficiency of the vessels can cause bad calf cramps at night. The good news is, there is a cure. In addition to vein ablation, massage therapy, acupuncture therapy, or intravenous hydration, the best treatment for leg cramps at night starts with treating the underlying vessel disease. This will prevent cramps and aching legs from happening.
Wellness and Pain Can Help
A range of options for treating a thigh cramp are available at Wellness and Pain. We offer conservative treatments, routine visits, and minimally invasive quick-recovery procedures. We can keep you free of problems by providing lifestyle education and home care advice to help you avoid and manage issues, quickly relieving the inhibiting lifestyle conditions when complications arise.
At Wellness and Pain, we personalize patient care plans based on each patient’s condition and unique circumstances to relieve pain, improve mobility and mental space, and improve your overall health.