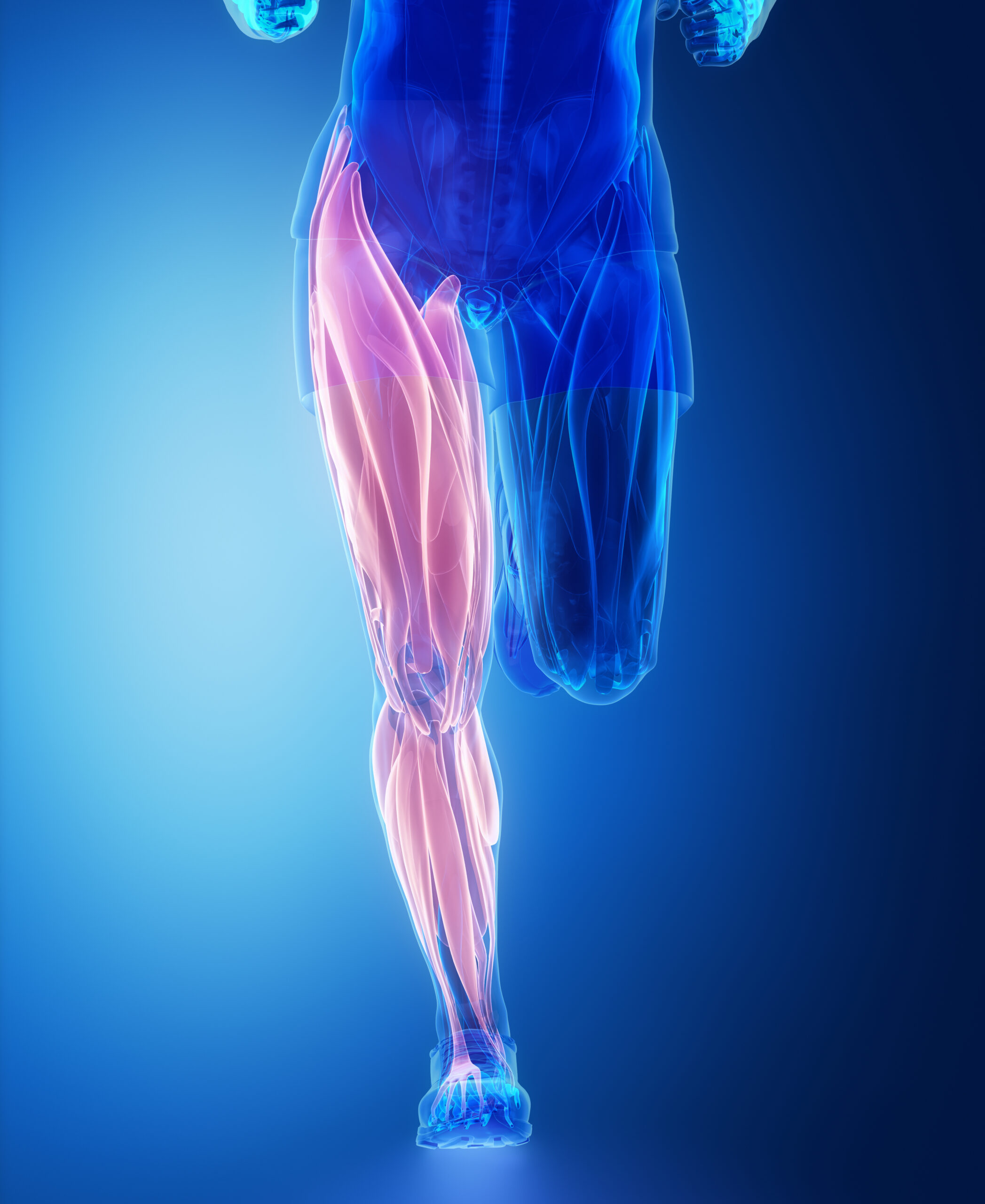
Due to their long and delicate nerves and blood vessels, your feet and toes are often the first to feel the brunt of diabetic foot pain.
Diabetes is known to cause damage to nerves and blood vessels because of the high levels of glucose in the blood. Diabetes and feet pain are two separate but related problems connected to the nerves and blood vessels in the feet. Combined, these two issues can cause diabetic leg pain and other foot complications — eventually warranting some sort of diabetic swollen feet treatment.
Diabetic Foot Pain, Blood Glucose, & Potential Infection
Blood sugar, or glucose, is too high when you have diabetes, which can eventually lead to diabetic foot pain. Food supplies you with glucose, and glucose is what fuels your cells. Glucose gets into your cells thanks to a hormone called “insulin.” Simply put, your body doesn’t produce enough insulin when you have Type 1 diabetes.
Type 2 Diabetes happens when your body doesn’t use or make insulin very well either. Cells cannot absorb glucose as fast if there’s not enough insulin being produced by your body. Glucose building up in your body causes high blood sugar levels.
Diabetes and feet pain can oftentimes go hand in hand. If you take care of your feet every day, you’ll be less likely to have diabetes-related foot problems, even if you’ve already lost a toe, foot, or leg because of it. Keeping your blood glucose levels low is important for your feet.
High blood sugar can damage a person’s feet over time. In diabetic neuropathy, nerve damage can cause numbness, tingling, pain, and loss of feeling in your feet. Diabetic neuropathy can prevent you from feeling cuts, blisters, or ulcers on your foot. As a result, you won’t know that they’re present. Thus, it can easily become infected. And because of the damaged blood vessels, your feet may not heal well.
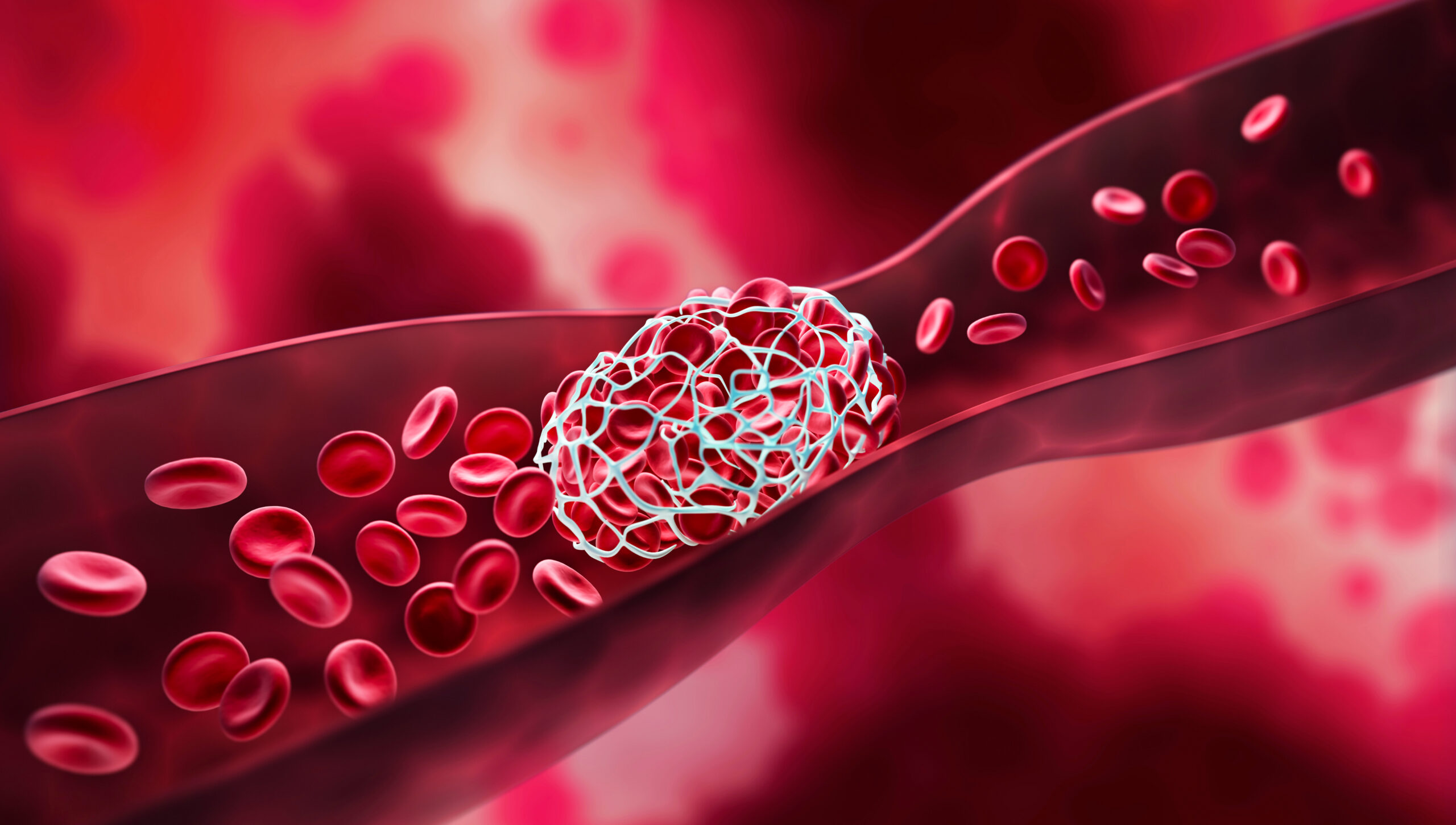
Your feet can also experience less blood flow when you have diabetes. Diabetic circulation problems are an unfortunate reality for many patients. You cannot heal a sore or an infection if you don’t have enough blood flow to your legs and feet. It’s possible for an infection to never heal. Gangrene may even result from the infection. Overall, diabetic foot pain is connected to everything mentioned herein.
Nerve Damage, Neuropathy, Arterial Disease & Diabetic Foot Pain
The nerve damage caused by diabetes, called “diabetic neuropathy,” can cause tingling and diabetic foot pain, making you lose your sense of feeling. Without feeling in your feet, you might not notice a pebble in your sock or a blister on your foot, leading to cuts and sores. Infected cuts and sores can be painful.
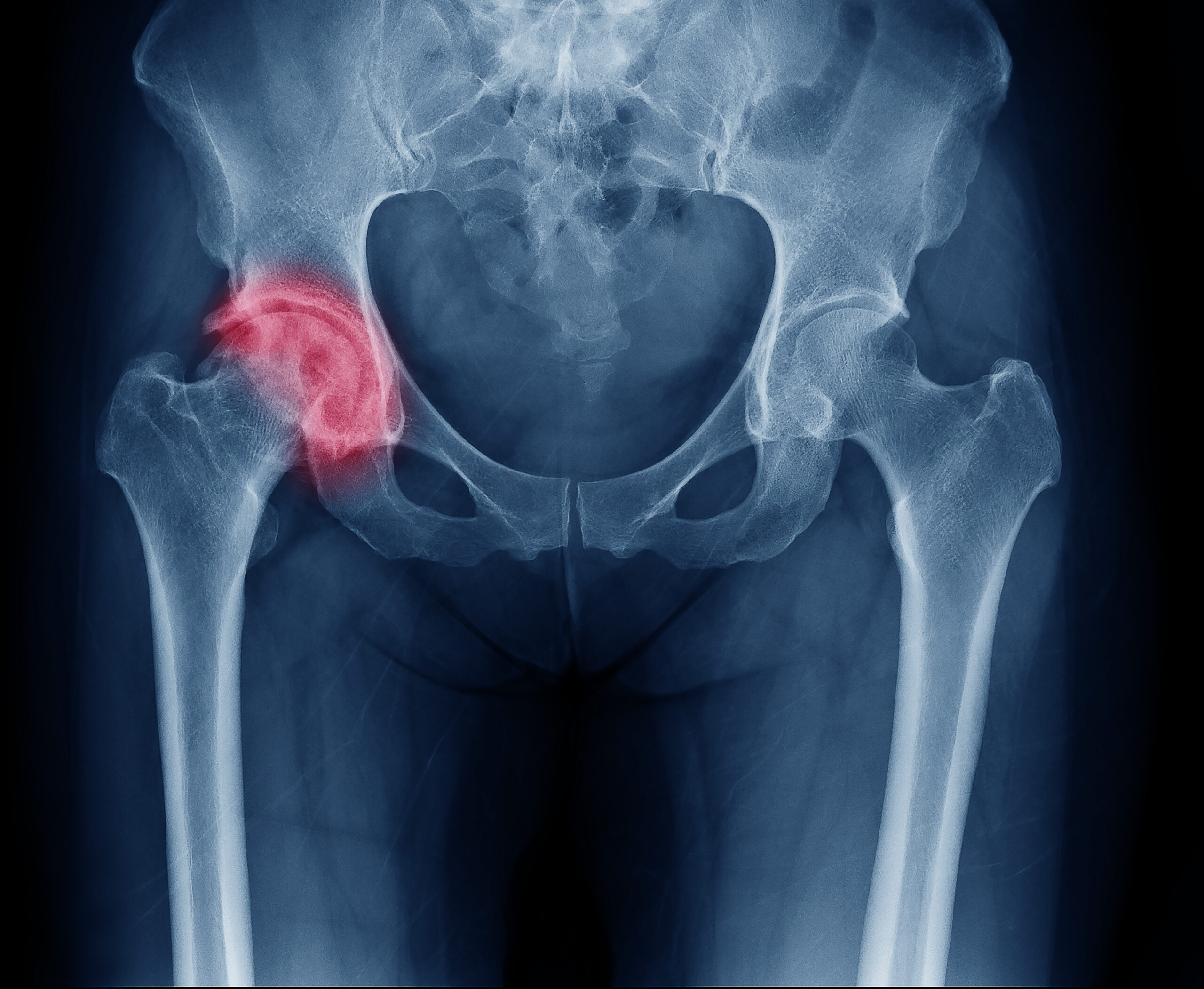
Diabetes can cause nerve damage leading to Charcot’s foot. Redness, warmth, and swelling are the first signs of Charcot’s foot, where your bones, joints, and soft tissue can gradually weaken in your lower extremities. Your feet can develop an odd shape later on if bones shift or break within your feet and toes.
Peripheral neuropathy causes numbness and pain in the feet and legs, making it hard to balance while walking. This is when nerves outside of the brain and spinal cord become damaged. Blood vessels become stiff and narrow after damage to their walls. As a result, the feet can receive less blood flow, resulting in a breakdown of the skin. There’s also a chance of infection, ulcers, and gangrene.
However, there’s a lot you can do to prevent diabetic foot pain and these other factors from worsening through treatment for diabetic neuropathy. You can take a proactive or defensive stance against your diabetes and feet pain problems.
What Does Diabetic Foot Pain Feel Like?
Symptoms of diabetic foot pain include:
- Injuries that take a long time to heal: Healthy blood vessels carry immune cells to fight infections and damaged tissue. Wounds take longer to heal if blood circulation is poor, which can and usually does happen with diabetes and materializes into formal diabetic circulation problems.
- Sensitivity or pain: Things that are normally not painful cause pain or sensitivity. Wearing certain socks can even hurt or feel uncomfortable when the material they are made of brushes against your feet.
- A bad tingling feeling: You feel like you’re on pins and needles. Your foot feels like it’s asleep.
- Numbness or weakness: Nerves tell your muscles what to do and they help you to feel things. You might have nerve damage if you don’t feel it when you step on an object or cut your foot. Numb feet are also more likely to get injured.
How Can I Protect My Feet?
Keeping your blood sugar levels under control is the best way to protect your feet and sliding into diabetic foot pain. By doing this, nerve and blood vessel damage has a better chance of not worsening. Keeping your feet’s skin healthy is the next step.
Checking your feet every day is part of good foot care for diabetics. Be on the lookout for cuts, redness, and other changes in the skin and toenails, including warts. Keep an eye on the bottoms of your feet too. Keeping your feet clean is also important. Make sure you’re using warm water and soap. You don’t want to soak your feet, because it can dry them out. Use cornstarch or something similar (maybe a powder) between your toes after drying your feet. Any moisture your feet may soak up can cause infections.
Using a clipper to trim your toenails straight across is good. You can have a podiatrist (foot doctor) trim your toenails if they’re thick or curve into the skin. It’s also important to ask your doctor how to remove corns and calluses safely. Thick skin can cause foot sores. You could damage your foot if you remove that skin in the wrong way. You don’t want to cut the skin or use medicated pads or liquids either.
Some Active Options
When walking, wear well-fitting shoes and socks or slippers to protect your feet. Even inside, you shouldn’t walk barefoot. Make sure your shoes are smooth inside. This will prevent you from being rubbed raw by a seam or a pebble. You’ll also be better off protecting your feet from heat and cold. At the beach, wear sunscreen and don’t go barefoot. Warm your feet with socks instead of a fireplace or heater in cold weather.
Lastly, when it comes to diabetic foot pain and Diabetic circulation problems, it’s important to keep blood flowing into your feet. Sit with your feet up. Throughout the day, wiggle your toes and circle your feet at the ankles. Socks shouldn’t be too tight. Walking is a good exercise that doesn’t hurt your feet. It’s important to get your feet checked at each of your healthcare visits. Getting your feet checked is a good idea even if you haven’t noticed anything wrong.
Diabetic swollen feet treatment could be your next resort if — for some reason — the above tips and tricks don’t work well in your particular circumstance. Diabetes and feet pain issues shouldn’t be ignored at any stage you happen to find yourself in. Modern lifestyle practices have helped many patients manage their pain and symptoms.
Can I Prevent Diabetic Foot Pain?
By managing your diabetes as well as you can, you can prevent or manage diabetic foot pain. High sugar levels cause nerve pain. Managing your blood sugar levels through diet, exercise, and medications can prevent diabetes complications.
It’s important to remember that diabetic foot pain isn’t just a nuisance, but can also be a sign of worsening diabetes. Managing diabetes requires regular foot exams performed by yourself and also with your doctor. Get your blood sugars in your target range so your foot pain doesn’t worsen. There are medications that can help if your foot pain persists despite lifestyle changes.
When Should I See a Diabetic Foot Pain Specialist?
Contact your health specialist right away to begin a healthy journey to curing your diabetic foot pain. Cuts, blisters, bruises, and skin that becomes red, warm, or painful on your foot might be signs of an infection.
Calluses with dried blood inside are often the first sign of a wound underneath. If you have a black and smelly foot infection, you might have gangrene, so take heed. Treatment for swollen feet diabetes is probably your best solution.
Wellness and Pain
When it comes to diabetic foot pain, you’re better off seeing a doctor who truly cares about you and your health. An evaluation may include a nerve conduction velocity and electromyography (NCV/EMG) test for nerve damage or a blood flow and circulation ultrasound for vascular disease.
Practitioners at Wellness and Pain confidently provide these important evaluations, apply their professional expertise, and offer the caring and sensitive diabetes and feet pain treatment you need to improve any symptoms you are experiencing.