Trigger point injections are a common treatment for muscle pain and discomfort caused by tight knots in your muscles called trigger points.
Understanding how it works and what to expect can ease your concerns about the procedure.
In this article, you’ll learn step-by-step the process so you feel informed and confident about your treatment.
What Are Trigger Point Injections?
Trigger point injections (TPIs) are a medical treatment designed to relieve pain by targeting specific areas of muscle tension known as trigger points.
These tight knots often cause localized discomfort and may also lead to referred pain, where it radiates to other parts of the body.
TPIs involve injecting a local anesthetic into the trigger point to alleviate pain and relax the affected muscles, aiding in overall trigger point management.
The whole process takes only a few minutes, and several trigger points can be addressed in a single visit.
After the injection, mild soreness or bruising may occur, but patients usually recover quickly. Ice or over-the-counter pain relievers can help with healing the affected area.
Doctors often recommend TPIs along with physical therapy or stretching exercises, especially when severe pain limits movement.
What Are The Benefits of Trigger Point Injections for Pain Relief?
If you deal with chronic muscle pain, trigger point injections are an ideal option for pain management.
Understanding the benefits of this treatment can help you make informed decisions about treating muscle pain.
Immediate Pain Relief
Trigger point injections quickly relieve muscle pain, especially when other treatments fall short.
Patients usually experience relief as soon as the local anesthetic, such as lidocaine, starts working. Sometimes, adding a corticosteroid helps reduce inflammation, providing even longer-lasting results.
People dealing with chronic muscle pain, tension headaches, or myofascial pain syndrome often feel significant improvement after treatment.
Quick and Non-Invasive Procedure
The procedure is quick and minimally invasive, taking less than 30 minutes, with little to no recovery time required. Patients can resume their regular activities right away.
Many choose trigger point injections over surgery because they don’t involve extensive recovery periods or significant downtime.
With such a fast turnaround, patients can focus on their routines without much interruption.
Long-Lasting Results
Relief from a trigger point injection can last from several weeks to a few months, especially when corticosteroids are included.
Patients often report significant pain reduction, allowing them to move more easily and engage in daily activities without discomfort.
For those managing chronic pain conditions, these injections can provide much-needed breaks from persistent pain.
Targeted Pain Management
The ability to target specific problem areas makes trigger point injections particularly useful for chronic conditions like fibromyalgia and myofascial pain syndrome.
The injections offer a localized approach, giving relief exactly where the pain originates, unlike oral pain medications that affect the whole body.
Minimal Side Effects
Trigger point injections come with very minimal side effects. Some patients experience slight soreness or bruising, but other than that, no serious side effects are associated with the procedure.
These symptoms usually go away on their own within a few days, and they rarely disrupt daily life.
Serious complications, such as infection or allergic reactions, are uncommon and usually avoided when proper procedures are followed.
Complementary to Other Treatments
Trigger point injections also work well alongside other treatments, such as physical therapy and exercise routines.
When combined, they offer a balanced way to address muscle pain and help patients regain mobility.
The injections allow patients to participate in rehabilitation or physical therapy more comfortably and speed up their overall recovery.
What Conditions Do Trigger Point Injections Treat?
The indications trigger point injections show are mostly for conditions such as myofascial pain syndrome, fibromyalgia, or persistent muscle tension.
The treatment is especially beneficial when trigger points lead to a referred pain pattern, where the pain is felt in areas distant from the trigger point itself.
- Myofascial pain syndrome: One of the most common conditions treated by TPIs is myofascial pain syndrome. For those experiencing persistent myofascial trigger point pain, TPIs can significantly improve mobility and reduce stiffness.
- Fibromyalgia and tension headaches: Patients with fibromyalgia, a condition that affects the soft tissues, also benefit from TPIs. These injections help treat myofascial pain caused by tender trigger points throughout the body, which are a hallmark of fibromyalgia. Similarly, tension headaches, often linked to trigger points in the neck and shoulders, can be alleviated by targeting these myofascial trigger points.
- Low back pain and sports injuries: Chronic low back pain frequently stems from myofascial trigger points in the muscles surrounding the spine. Injecting medication directly into the affected areas provides targeted pain relief and helps restore normal muscle function.
- Muscle Spasms: Persistent, painful muscle contractions, often in the back or neck, that do not relax on their own, can be alleviated through TPIs.
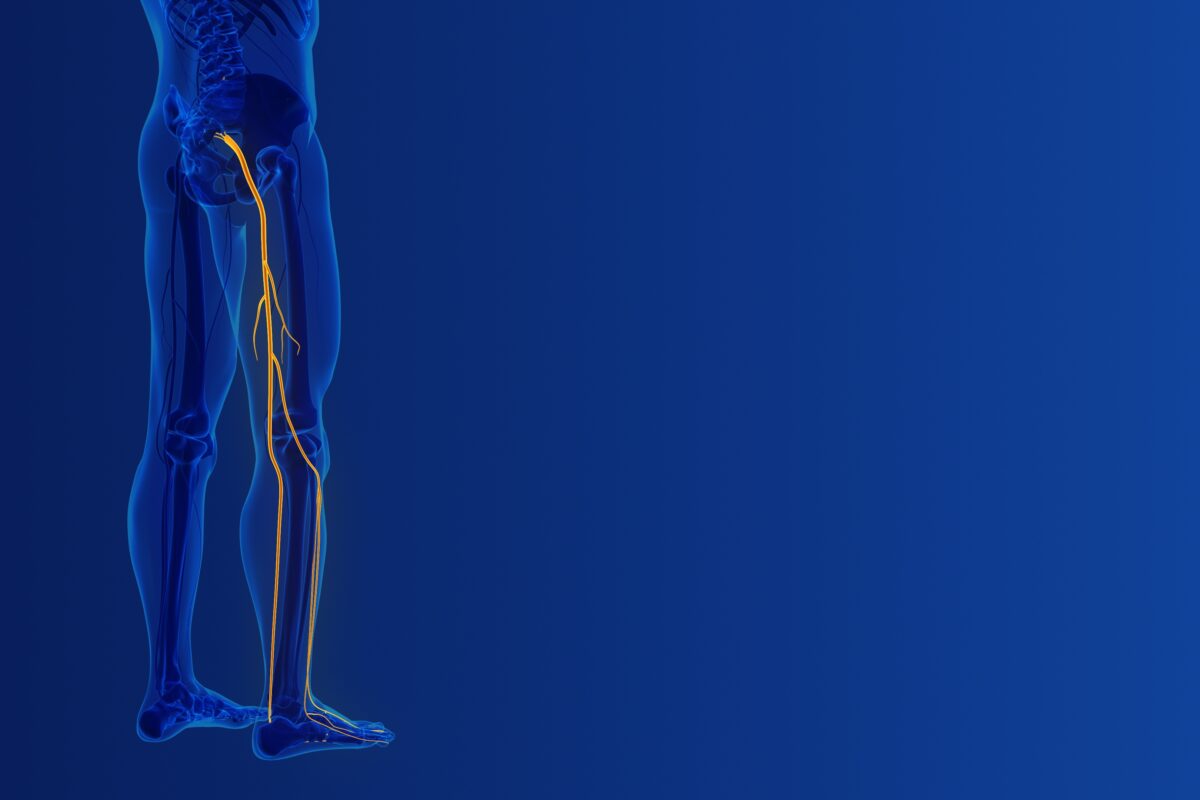
Sciatica pain relief: Trigger point injections can effectively target specific muscle knots or “trigger points” that can cause nerve compression and radiating pain down the leg, providing immediate sciatica pain relief.
What to Expect During Trigger Point Injections
Trigger point injections are a relatively quick and safe procedure. But of course, it’s important to familiarize yourself with the procedure to help manage your expectations before, during, and after the injections are administered.
Here’s what you need to know:
Before Trigger Point Injections
Before receiving trigger point injections, patients will typically have a consultation with their healthcare provider to assess their condition.
During this initial assessment, the physician will review the patient’s medical history, current symptoms, and areas of pain.
They may ask questions to pinpoint the location and severity of the trigger points. The provider might also conduct a physical examination, palpating the muscle areas to identify the problematic knots.
Patients are advised to inform their healthcare provider of any medications they are currently taking, including blood thinners, as these might need to be adjusted before the procedure.
Allergies to any medications or anesthetics should also be mentioned to avoid any adverse reactions during the injection.
Some patients may be asked to avoid strenuous physical activity or massage therapy the day before the procedure, while others may be advised to use ice or heat packs on the area beforehand to reduce discomfort.
During Trigger Point Injections
The actual procedure for trigger point injections is typically quick and minimally invasive. Patients will be asked to either sit or lie down, depending on the location of the trigger points being treated.
The healthcare provider will clean the injection site to maintain a sterile environment and may apply a topical anesthetic to reduce discomfort.
Using a small needle, the physician injects a local anesthetic, saline, or corticosteroid directly into the trigger point.
This process relaxes the muscle knot and alleviates pain. In some cases, dry needling (where no medication is injected) stimulates the muscle and releases tension.
You may experience a local twitch response, which signals the muscle’s reaction to needle contact with a trigger point. Muscles contract involuntarily when the needle stimulates the taut band, showing that the sensitive area has been properly targeted.
The entire procedure typically takes only a few minutes, and multiple trigger points can be addressed in one session if needed.
After Trigger Point Injections
After the injections, patients may experience some mild soreness or bruising at the injection site. This is a normal reaction and usually subsides within a few days.
Most healthcare providers recommend resting the treated area for 24 to 48 hours after the injection, though light activity, such as walking, is typically encouraged to prevent stiffness.
Ice packs can be applied to the injection site to reduce any swelling or discomfort. Over-the-counter pain medications, such as ibuprofen, may also be recommended if needed.
However, patients should avoid strenuous physical activity or heavy lifting for at least a day or two post-injection.
Many patients notice an immediate reduction in pain and muscle tightness following the procedure, although it may take a day or two for the full effects to become apparent.
For chronic conditions, repeated injections might be required over time, based on the patient’s individual response to the treatment.
What to Look For in A Provider For Trigger Point Injections
When looking for a provider for trigger point injections, focus on a few key aspects to ensure you’re getting the care you need. Wellness and Pain serves as a great example of what to expect:
- Active pain management approach: Look for a clinic that takes an active approach to treating your pain. Wellness and Pain offers a variety of treatments, from simple therapies to more advanced, minimally invasive injections. Their team tailors treatments specifically to your health condition, aiming for the best results.
- Experienced specialists: Seek a clinic led by knowledgeable doctors. Wellness and Pain is staffed by experienced specialists who attend to conditions such as chronic pain and muscle tension, ensuring you’re in capable hands.
- Diverse condition treatment: Choose a provider that treats a range of issues. Wellness and Pain specializes in addressing various conditions, including back pain, sciatica, and fibromyalgia. Their trigger point injections specifically target areas of discomfort, giving patients targeted pain relief.
- Insurance transparency and accessibility: A good clinic will be upfront about insurance coverage. Wellness and Pain accepts most major insurance plans and has several convenient locations across New Jersey and New York, which makes accessing care easier.
- Patient-centered care: A clinic that focuses on long-term health is important. Wellness and Pain provides advice on home care and lifestyle adjustments to help prevent future pain, showing that they prioritize long-term wellness over temporary relief.
Why Wellness and Pain is the Right Choice for Trigger Point Injections
At Wellness and Pain, we understand how debilitating chronic muscle pain, spasms, and tension can be.
We believe that choosing the right place for your trigger point injections is key to getting the relief you need, and we’re confident we can provide that relief.
Here’s why you should choose us for getting trigger point injections:
Our Expertise in Pain Management
Our team specializes in pain management, and we’ve spent years helping people just like you overcome various pain conditions. We don’t offer one-size-fits-all solutions.
Instead, we take the time to evaluate the underlying cause of your pain, ensuring that we target the exact area that needs relief.
You’ll get focused, precise treatment that addresses your unique situation, not just temporary fixes.
Tailored Care for Every Patient
At Wellness and Pain, we treat you as an individual. We don’t believe in generic treatments because we know that each person’s pain is different.
When you come to us, we’ll carefully assess your medical history, lifestyle, and specific pain areas.
We’ll then craft a personalized treatment plan that addresses your needs, providing you with the best possible path toward relief.
Precision Through Advanced Technology
When it comes to trigger point injections, precision matters; that’s why we use the latest technology, including ultrasound guidance, to make sure your injections go exactly where they need to.
Our advanced tools help us hit the right spot, reducing the risk of complications and speeding up recovery. You’ll get the targeted relief you’re looking for without the guesswork.
Compassionate Care You Can Trust
We know pain isn’t just physical. It affects your mental well-being, too, and we’re here to support you every step of the way. From the moment you walk into our clinic, you’ll notice that we’re different.
We listen to your concerns, answer your questions, and make sure you’re comfortable throughout your entire treatment. We’re here to help you not only physically, but emotionally as well.
Holistic Approach to Long-Term Wellness
At Wellness and Pain, we don’t just aim for short-term relief.
Our approach focuses on your overall wellness, combining trigger point injections with other therapies like physical therapy, lifestyle adjustments, and stress management.
Get Trigger Point Injections Today With Wellness and Pain
Find relief from chronic muscle pain with Wellness and Pain’s trigger point injections. Our skilled specialists target pain points directly to reduce your discomfort and manage your pain better.
We offer personalized care that addresses your specific needs so you can focus on enjoying life and take charge of your overall health.
Call us at (844)-949-2358 or fill out this form for more information.
FAQ About Trigger Point Injections
What are trigger point injections?
Trigger point injections offer relief for muscle pain caused by knots or tight spots, known as trigger points. A small dose of anesthetic or saline goes directly into the problem area, relaxing the muscle and reducing pain.
How do trigger point injections work?
The injection interrupts the nerve signals that cause muscle knots, helping the muscle to release tension and pain. Blood flow improves in the area, which helps the muscle recover.
Are trigger point injections safe?
Trigger point injections carry minimal risks when handled by trained professionals. Common side effects include mild soreness or bruising, but serious reactions rarely occur.