Knee Pain: Causes, Limitations, & Treatment
While injuries, osteoarthritis, rheumatoid arthritis, aging, and other life circumstances can all lead to knee pain, any comprehensive pain management plan should aim to improve recovery and reduce discomfort.
For optimal results, pain management experts usually utilize a combination of pain relief options. Individual treatments may not seem to make a difference at first, but when used in conjunction with other methods, they can produce the successful results you’re looking for. Chronic and persistent pain issues can cause flare-ups any time of the day or week, which makes it difficult to walk and perform normal tasks. Maybe you’re experiencing pain when you bend your knees, place weight on them, or even just sit, stand, or relax.
These intense pain problems can be alleviated or eliminated through a number of ways, giving you an effective cure for a long-term solution — and most importantly, the hope you need to live healthier. The most effective way of dealing with pain is to see a pain management specialist or doctor. These experts are highly trained to develop customized treatment plans for their patients.
Knee Pain Causes, Associations, & Factors
Almost everyone experiences knee pain at some point in their lives. In the United States, nearly 25 percent of adults endure it at some point. What’s more: it can be caused by a number of different factors. The following are some of the most common associations:
- An injury, such as a sprain, strain, or fracture.
- The overuse of the knees from running or playing sports.
- Arthritis of the joints that is caused by an autoimmune disease — namely rheumatoid arthritis.
- The cartilage in the knee starts breaking down due to osteoarthritis, a form of arthritis.
On a sliding scale, there’s a wide range of pain severity. A severe knee injury can make it difficult to walk or participate in activities, making it worth the effort to seek treatment.

Fortunately, patients have a variety of options to treat the pain and discomfort. They include medication, exercise, and surgery. Pain relievers, anti-inflammatory drugs, and over-the-counter pain relievers can be used. However, some patients choose an orthopedic surgeon to treat bone problems, joint problems, ligament problems, tendon problems, and muscular problems. Rheumatologists can also treat diseases that cause joint pain in addition to arthritis.
Knee Pain Treatment
Fortunately, patients have a variety of options to treat the pain and discomfort. They include medication, exercise, and surgery. Pain relievers, anti-inflammatory drugs, and over-the-counter pain relievers can be used. However, some patients choose an orthopedic surgeon to treat bone problems, joint problems, ligament problems, tendon problems, and muscular problems. Rheumatologists can also treat diseases that cause joint pain in addition to arthritis.
Exercises and stretches, movement training, and massage therapy can increase mobility, ease pain, and prevent further damage as well. Sharp knee pain may be relieved or cured with these treatments. As a result, muscles around the knee can be strengthened and more flexible, thereby improving your knee’s function. Routine exercises can also improve mobility and function. The knees should be exercised in a way that does not overstrain them.
When other treatments fail to relieve severe pain, it can be worth consulting a specialist. Acute pain can become chronic pain when it lasts for more than a few months. Unfortunately, chronic pain usually persists for longer periods than you’d expect.
In either case, you should consult a pain management specialist for diagnosis and treatment. Whoever you consult, your specific condition should always be taken into account when developing a customized plan for a successful, healthier you.
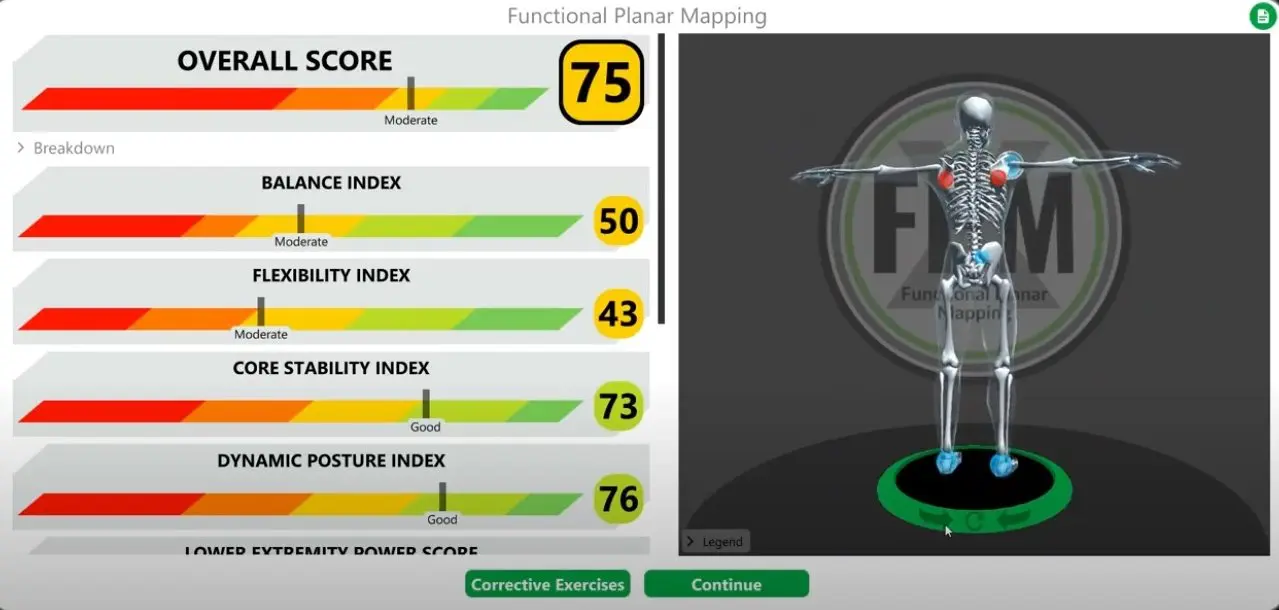
Comprehensive Diagnosis and Treatment for Knee Pain
Effective management of knee pain begins with a thorough diagnosis. Diagnostic options for knee pain can include:
- X-ray of the knee: This imaging test can reveal bone abnormalities, fractures, and alignment issues in the knee joint.
- MRI of the knee: MRI scans provide detailed images of soft tissues, such as muscles, tendons, and ligaments, helping to identify issues like cartilage damage or inflammation.
- Ultrasound of the lower extremities: This test examines vascular causes of pain, such as blood clots or poor circulation, which can contribute to knee discomfort.
Wellness and Pain Can Help
A range of options are available at Wellness and Pain to treat your knee pain. We offer chiropractic massage, routine visits, and minimally invasive quick-recovery procedures. Minimally invasive treatments include stem cells, vein ablation, and microarthroscopy. We can keep you free of problems by providing lifestyle education and home care advice to help you avoid and manage issues, quickly relieving the conditions inhibiting your life.
At Wellness and Pain, we personalize patient care plans based on each patient’s condition and unique circumstances to relieve pain, improve mobility and mental space, and improve your overall health.
Treatments for Knee Pain
Other knee surgeries
Other knee surgeries
...
Knee reconstruction
Knee reconstruction
...
MCL repair
MCL repair
...
Meniscal tear
Meniscal tear
...
Trigger Point Injections
Joint Pain Relief Injection
Joint Pain Relief Injection
Joint pain relief injections, such as corticosteroids or hyaluronic acid, are used to reduce inflamm...
Epidural for Neck and Back Pain
Epidural for Neck and Back Pain
...
Medial Branch Blocks
Medial Branch Blocks
...
Nerve Ablations
Nerve Ablations
...
Injections for Migraines
Injections for Migraines
...
Arthroscopy
Arthroscopy
...
NCV/EMG
NCV/EMG
...
Nerve Conduction Velocity
Nerve Conduction Velocity
...
Trigger Point Injections
Trigger Point Injections
TPI are used to treat painful and tender areas of muscle. They are intramuscular and subcutaneous in...
Vein Ablation
Vein Ablation
Vessel ablation – formally known as radiofrequency ablation (RFA) – is a minimally invasive and ...
Massage Therapy
Massage Therapy
Pain including Muscle Tension, Back and Shoulder pain, Repetitive stress injuries, Headaches, Neck p...
Acupuncture Therapy
Acupuncture Therapy
A traditional Chinese medicine technique that is used to stimulate energy flow and promote healing. ...
Chiropractic Services
Chiropractic Services
Flexion-distraction therapy is a specific gentle technique performed on a segmented table that moves...