Hip and leg pain can mean much more than just old age or being out of shape, with the causes falling into four main categories. These include problems with joints and movement, blood flow issues in arteries, nerve issues often from blood clots, or troubles with veins.
Picture someone who runs every day whose joint pain creeps in slowly, not because of one clear injury, but as a slow buildup. From so many miles, their labrum or cartilage gets tiny tears, yet what truly hurts them isn’t just the ache, but the inability to run, which impacts their very sense of self.
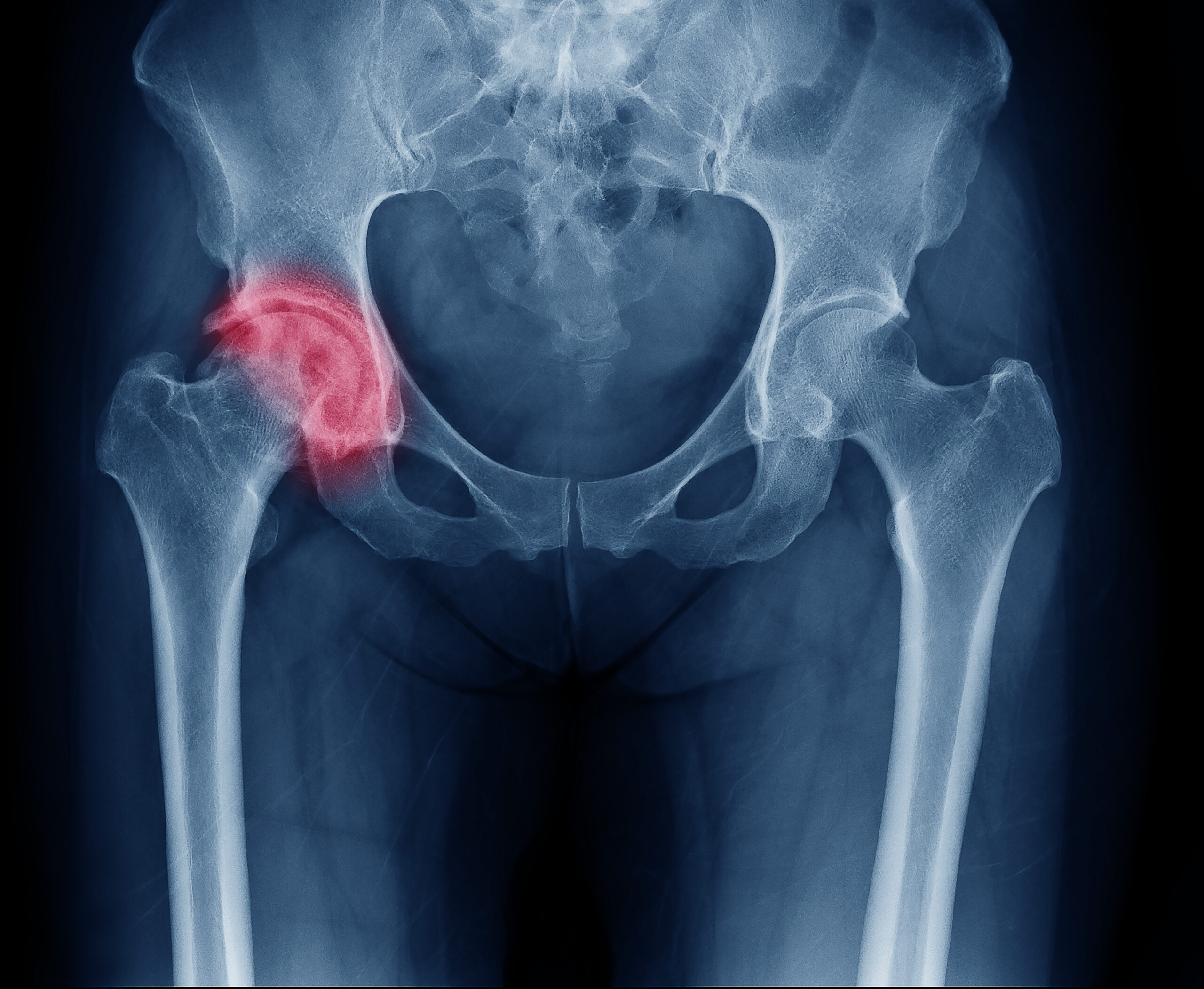
Osteoarthritis isn’t just joints getting old. The main tissue, cartilage, breaks down from an uneven war between the things that build it up and the things that eat it away. As a result, the space between bones gets tighter and bone spurs pop up, while the classic pain feels deep, often in the groin or upper thigh.
Blame the nerves for where the pain shows up, which causes many people to instinctively grab their hip in a C-shape when showing doctors where it hurts. There’s a sharp stiffness when they move after sitting still, and trying to turn the leg inwards is tough, which is usually the first movement to go.
Early damage doesn’t always show up on an X-ray. Softer tissues like the labrum often need an MRI to show the real story, after which doctors use a system called Kellgren-Lawrence to rate how much space remains in the joint.
A sore hip changes how someone walks, causing them to limp to avoid pain, and that limp uses a lot more energy — sometimes a third more than normal. This limp can throw off other muscles and joints, resulting in tight hip flexors, aching backs, weakened outer hip muscles, and knees tracking out of line. While the pain may travel, the original problem started at the hip.
If the hip is the root cause, trying to fix knee pain or calf aches won’t help. It’s smarter to work on the surrounding muscles before things get severe. While painkillers are helpful, drugs like Duloxetine sometimes work better for nerve pain, and some people try injections using their blood’s platelets or stem cells to calm down the whole joint.
Ultimately, hip replacement surgery comes as a last step, not just based on the X-ray. For these patients, daily life has become too tough.
“It is not always known what causes the lack of blood supply,” states OrthoInfo. “But doctors have identified a number of risk factors that can make someone more likely to develop osteonecrosis: injury, excessive alcohol use, corticosteroid medicines, and medical conditions.”
A Senior’s Vascular Emergency: Hip and Leg Pain
Peripheral Artery Disease (PAD) isn’t just a hip and leg pain issue. It’s like a flashing red light for deeper artery problems all over the body.
Many brush off leg pain, thinking it’s just exhaustion or old age. In truth, these aches can be a clue that blood isn’t flowing well, especially in smokers or those with high blood pressure.
The most common complaint is a cramp in the calf, although that pain can show up in the thigh or buttocks too. People usually notice it after walking the same distance each time — maybe 100 yards — when the cramp forces them to stop, yet after a short rest, the pain vanishes until they start walking again. This happens because poor blood flow causes the muscles to get less oxygen, allowing acid byproducts to build up and trigger pain.
Doctors use the Ankle-Brachial Index, or ABI, to spot PAD. This quick check compares ankle blood pressure to arm blood pressure. If the reading is under 0.90, that points to PAD, but a drop much lower (near 0.40) means the arteries are dangerously blocked.
Tests like Duplex Ultrasound help pinpoint the problem spots, and if surgery might help, 3D scans like CTA or MRA map the arteries. Sometimes, PAD gets so bad that wounds stop healing, which is a medical emergency requiring swift treatment to restore blood flow.
PAD affects more than pain, as the lower leg muscles can shrink over time from poor circulation. You might notice thinner hair, shiny skin, or toes that take a while to flush pink when pressed, and while the body tries to grow new small vessels around blockages, this doesn’t always work. If the tissue is starved too long, it can die, and a diagnosis of PAD signals a much higher chance of heart attack or stroke.
“Many people with PAD have no symptoms,” according to the National Health Service. “However, some develop a painful ache in their legs when they walk, which usually disappears after a few minutes’ rest. The medical term for this is ‘intermittent claudication.’ The pain can range from mild to severe, and usually goes away after a few minutes when you rest your legs. Both legs are often affected at the same time, although the pain may be worse in one leg.”
Treatment needs a full-court press, including high-dose statins to lower cholesterol and blood thinners like Aspirin or Clopidogrel to prevent clots. Doctors may also use medications like Cilostazol to help with pain, but the most important step is quitting all tobacco now because lifestyle change matters most.
Structured walking improves symptoms by forcing new tiny vessels to grow, but sometimes fixing the arteries means balloon procedures or stents. Other times, surgery with a bypass graft is needed. Sticking with a treatment plan can make all the difference.
The Desk Worker’s Danger: Deep Venous Thrombosis
Sitting for hours is just plain uncomfortable, and it’s sometimes a sign of underlying hip and leg pain problems. It can set off a chain of events in your body that leads to Deep Vein Thrombosis, or DVT.
This condition happens when blood thickens and forms a clot deep in your leg veins, putting people working from home, frequent fliers, or anyone stuck in bed after surgery all at risk. Lack of movement is a big culprit.
Doctors describe three major triggers for DVT:
- Not moving slows blood flow.
- The blood sometimes becomes stickier and clots more easily.
- Injury to the inside walls of your veins can help a clot form.
A person usually feels pain strongly and unyieldingly on one side of the leg, mostly in the calf, and though moving the foot upward can sometimes worsen the pain, that sign alone can’t be trusted. Swelling, redness, and warmth in your leg should raise a red flag.
The real worry with DVT is that a piece of the clot might break off and lodge in the lungs, a condition known as a pulmonary embolism. Doctors use a system called the Wells Prediction Rule to judge risk, with high scores calling for immediate scans, while a blood test called a D-dimer helps rule out clots if results come back negative.
However, the go-to for diagnosis is an ultrasound. If the technician pushes on the vein with the probe but it doesn’t compress, that signals a clot is blocking the way.
There’s an extra risk if the clot sits up higher in the pelvis, especially in bigger veins near the hip, which can lead to more serious complications, like a large clot shooting up to the lungs or long-term issues with blood flow. Sometimes doctors will use clot-busting drugs for these higher risk cases, so sudden, unexplained pain in the groin or hip after sitting for hours needs the same fast work-up as a swollen calf.
Once DVT is suspected, treatment starts right away with blood thinners, with pills like Rivaroxaban and Apixaban now common. For DVTs linked to a clear cause, three to six months of treatment is typical, but some people need blood thinners indefinitely if their DVT keeps returning or no cause is found.
To help your leg heal and reduce the chance of lingering pain and swelling, doctors recommend wearing compression stockings. This might be needed for up to two years.
The bottom line is that prolonged sitting can trigger a dangerous chain reaction in your legs. Small breaks, movement, and listening to your body go a long way. If your leg swells suddenly or aches deep within, don’t brush it off, because action today can stop a small problem from turning into something deadly tomorrow.
Hip and Leg Pain and CVI for Standing Professionals
Spending hours on your feet wears down your legs, causing hip and leg pain. It doesn’t take much wear and tear for Chronic Venous Insufficiency (CVI) to set in if your veins can’t keep up.
Over time, the one-way valves deep inside the legs start to falter, causing blood to slip backward, gather in the lower legs, and leak fluid and red blood cells out, resulting in swelling around the ankles by evening.
You know the feeling when your legs ache deeply, feel heavy, and become restless, yet propping your feet up makes the ache fade fast. The skin around your ankles might even start to change color, showing a rusty brown stain, and sometimes the skin grows thick and tight like old leather, which is why doctors use the CEAP scale to rate how bad it gets (Clinical Class, Etiology, Anatomical, Pathophysiology).
Finding out for sure means a special ultrasound, where doctors check how long blood sneaks back in the veins when you stand. If it takes half a second or more, that’s a big clue.
CVI is not just a leg problem, as it sometimes stretches up to the pelvis, especially in women after childbirth, causing stubborn pain deep in the hips or pelvis. The issue is hidden reflux in veins around the ovaries or pelvis, and diagnosing this form of vein trouble often calls for high-tech scans like special CT or ultrasound from inside the vein.
“Hip pain that radiates down the leg can be caused by multiple mechanisms within the hip joint, SI joint, or the muscles, tendons, and nerves in this area,” states VeryWell Health. “Possible causes include sciatica, arthritis, bursitis, GTPS, labral tear, endometriosis, and more. Treatment will depend on what is causing your hip pain so it’s important to get a proper diagnosis.”
Treating these problems starts simple: strong compression stockings help veins push blood the right direction, and walking helps squeeze the calf muscle to send blood upward. Additionally, lifting your legs above your heart three times each day for half an hour pulls swelling down.
If the main leg veins are leaking, doctors often seal them shut with a laser or heat probe or use glue, while in pelvic vein problems, tiny coils block off the leaking part during a short procedure. Tackling leg pain from standing starts with moving, good socks, and giving your legs time to rest.
If that isn’t enough, newer fixes can seal the trouble at its source.
Four Pathways of Lower-Extremity Pain
Here’s a summary on the differentiators of chronic hip and leg pain, from cause and symptom pattern to diagnosis and urgency – described in scenarios:
| Feature | Hip Osteoarthritis (OA) | Peripheral Arterial Disease (PAD) | Deep Vein Thrombosis (DVT) | Chronic Venous Insufficiency (CVI) |
| Primary Cause | Mechanical failure (Cartilage degradation, micro-trauma) | Arterial failure (Atherosclerosis/Plaque-limited flow) | Thromboembolism (Virchow’s Triad: Stasis/Clotting) | Valvular failure (Venous reflux/Venous Hypertension) |
| Cardinal Symptom | Deep Groin Pain (C-sign); Gelling (stiffness after rest); restricted rotation. | Intermittent Claudication (Predictable cramp with walking); stops completely with rest. | Sudden, Unilateral throbbing, constant ache, heat, and severe Edema. | Heavy, tired, restless ache; Worse with standing/sitting; Relieved by elevation. |
| Pain Mechanism | Loss of joint space/Synovitis | Oxygen demand deficit (Ischemia) | Obstructed venous return/Inflammation of vein wall | High hydrostatic pressure in capillaries |
| Diagnostic Test | Radiographs (Kellgren-Lawrence Grading); MRI with Contrast. | Ankle-Brachial Index (ABI); Duplex Ultrasound Mapping. | Compression Venous Duplex Ultrasound; D-dimer blood test. | Duplex Ultrasound Reflux Study (patient standing). |
| Urgency and Risk | Chronic, functional loss; Antalgic gait leading to compensatory pain. | High systemic risk (MI, Stroke); Risk of Critical Limb Ischemia (CLI). | ACUTE MEDICAL EMERGENCY (High risk of Pulmonary Embolism (PE)). | Chronic, progressive risk of skin changes (Hemosiderin), Post-Thrombotic Syndrome (PTS), and ulcers. |
| Management | Prehabilitation (PT); NSAIDs/Duloxetine; Ultimate THA (Hip Replacement). | Nicotine Cessation; Supervised walking; Statins; Revascularization (Stent/Bypass). | Immediate Anticoagulation (DOACs); Mandated Compression Stockings (for 2 years). | High-grade Compression Therapy; Leg Elevation; Definitive Endovenous Ablation. |
Hip and Leg Pain Questions and Answers
Symptom varieties, urgency, and treatment remain common concerns for hip and leg pain patients. Here are our expert answers to some of your most pressing hip pain and leg pain questions:
What is the absolute definitive clinical test to rule out a vascular emergency like DVT or severe PAD?
- To Rule Out DVT: A negative D-dimer blood test in a patient with a low or moderate Wells Score is highly effective (over 95 percent sensitivity) at ruling out acute DVT, often making an ultrasound unnecessary. If the D-dimer is high, a Compression Venous Duplex Ultrasound is required.
- To Rule Out Severe PAD: An Ankle-Brachial Index (ABI) calculation. An ABI less than 1.0 is normal, while values approaching 0.40 or lower indicate severe arterial insufficiency requiring immediate intervention.
Is there a specific medication that targets the joint pain in OA without being an NSAID?
- Yes. Duloxetine (Cymbalta), an antidepressant, is FDA-approved for chronic musculoskeletal pain, including OA. It works centrally by modulating pain pathways in the brain and spinal cord, offering an alternative when NSAIDs are contraindicated (due to kidney or gastrointestinal issues). Additionally, Tanezumab, a monoclonal antibody that targets Nerve Growth Factor (NGF), is a novel biologic currently under investigation for refractory OA pain.
Why does walking through the pain help PAD but resting/elevation helps CVI?
This difference highlights the core pathophysiology:
- PAD (Arterial Ischemia): Walking forces the body to adapt to an oxygen deficit. This controlled stress stimulates the creation of new small blood vessels (collateral circulation), effectively providing natural bypasses around the blockage.
- CVI (Venous Hypertension): Resting/Elevation reduces the hydrostatic pressure. When the leg is elevated, gravity assists the failing valves by draining the pooled blood, resolving the venous hypertension that causes the aching and swelling.
My hip pain gets worse when I stand for a long time, but also after I sit. Is this OA or something else?
This combination suggests mixed pathophysiology:
- Pain after sitting (Gelling): Highly suggestive of Hip OA.
- Pain after prolonged standing: Highly suggestive of Venous Congestion (PCS or CVI) or severe lumbar spine stenosis (neurogenic claudication).
A physician needs to perform both orthopedic tests (for OA) and a specialized Venous Duplex Ultrasound (for CVI/PCS) to differentiate.
Additional Q&A: Blockage, Compression Stockings, and More
How do doctors decide whether to treat a PAD blockage for hip and leg pain: with a stent or open surgery?
This is determined by the length and location of the lesion, a vascular surgery decision based on the TASC II classification (TransAtlantic Inter-Society Consensus).
- Short, Focal Lesions: Often treated with minimally invasive endovascular therapy (balloon angioplasty and stenting).
- Long, Complex, or Occluded Lesions: Often require durable, open bypass surgery (femoropopliteal bypass) using the patient’s own vein or a synthetic graft. The goal is to maximize long-term vessel patency.
If I have had a DVT, how long do I really need to wear the compression stockings?
- Current authoritative guidelines recommend wearing graduated compression stockings for at least two years following a proximal DVT. This long duration is necessary because the benefit lies in preserving the remaining vein valve function and dramatically reducing the incidence and severity of Post-Thrombotic Syndrome (PTS).
Can a herniated disc (Sciatica) be mistaken for any of these four conditions?
- Yes, especially for hip OA. Sciatica (nerve pain from the back) causes electric, shooting, or tingling pain down the leg. The key difference is the quality of the pain. If it’s a mechanical ache (stiffness/gelling), think joint (OA). If it’s a nerve shock or tingling, think spine. An MRI can decisively separate the two.
Why is my hip pain actually felt in my groin, and not on the side of my hip?
- This is a critical distinction that saves time. True pain originating from the hip joint itself (OA) is felt deep in the groin, inner thigh, or sometimes the knee. Pain felt strictly on the outside (lateral) hip is usually from the soft tissues (like trochanteric bursitis) or the muscle tendons.
What are the primary lifestyle changes for CVI that are more effective than medication?
The most effective “treatments” are mechanical:
- Calf Muscle Pump Activation: Regular walking or heel raises to maximize the pumping action of the calf muscles, which squeeze blood out of the deep veins.
- Weight Management: Reducing body mass index (BMI) significantly lowers abdominal pressure on the major pelvic veins.
- Positional Drainage: Elevating the legs above the heart level three times a day for 30 minutes.
DVT feels like an emergency. What signs require an immediate emergency room visit?
- Any sudden, severe, one-sided pain and swelling is a medical alert. Don’t hesitate if the leg feels warm, tender, or red. The highest risk sign is having these symptoms combined with shortness of breath or chest pain — this could mean a life-threatening Pulmonary Embolism (PE). Stop searching online and go to the ER immediately.
Wellness and Pain
Find your personalized hip and leg pain treatment by visiting Wellness and Pain. We offer conservative treatments, routine visits, and minimally invasive quick-recovery procedures. We can keep you free of problems by providing lifestyle education and home care advice.
This enables you to avoid and manage issues, quickly relieving your inhibiting lifestyle conditions when complications arise. We personalize patient care plans based on each patient’s condition and unique circumstances. Wellness and Pain can help improve wellness, increase mobility, relieve pain, and enhance your mental space and overall health.