Before the age of dental sleep devices, treating Obstructive Sleep Apnea meant using a CPAP machine or ignoring the problem.
Things have changed. Doctors now see sleep problems as bigger health issues, with entire teams handling these cases now.
Pain management specialists, doctors, and dentists combine their knowledge, all aiming for one thing: better health for patients. Each person plays a part, and safety comes first.
The team checks that any dental device works well. Today, they all want each patient to feel better for years to come.
“Obstructive sleep apnea (OSA) remains largely underdiagnosed although highly prevalent, partly attributable to fragmented care delivery across disconnected primary, pulmonary, dental, and psychological providers,” according to a study published in Preprints. “Primary clinicians are responsible for evaluating the risk of obstructive sleep apnea (OSA) and making referrals for sleep testing. Sleep specialists validate diagnoses and devise individualized treatment strategies that may include positive airway pressure devices, oral appliances, or surgery.”
Take a Ride on the Sleep Apnea Care Circle
A sleep doctor’s team can lead the way, diagnosing your problem and recommending a quality dental sleep device. That’s a relief, given the fact that finding out you have sleep apnea can feel overwhelming.
You suddenly become the main focus of a team built just for your needs, where each person in the group has a clear role. They figure out exactly how serious things are, sometimes using a measure called the Apnea-Hypopnea Index (AHI). They choose what treatment makes sense for you — an oral mouthpiece, or CPAP, or sometimes surgery.
Sometimes, a specially trained dentist works on your jaw and mouth. This isn’t just any dentist – they’ve learned how jaws, breathing, and the rest of your body connect. They craft and adjust custom mouthpieces for people who can’t use other machines at night. Their goal is your goal: better sleep without discomfort.
A sleep technician runs the tests, which might happen in a lab or at home. They check your oxygen and track your brain waves. Those test results guide everyone else in making smart choices for your care.
A primary care doctor keeps watch on everything else, checking your blood pressure and watching for problems like diabetes or heart issues. Untreated sleep apnea makes those even worse, so this doctor ties all the pieces together.
With this circle around you, support comes from every side. You gain a team that watches every detail to help you sleep better and feel better each day.
How Referrals and the Dental Sleep Device Network Work Together
Collaborative care bridges every personal circumstance to catch every dental sleep device patient that needs help. Instead of handing out mouth guards, this process works like a conversation between doctors and dentists.
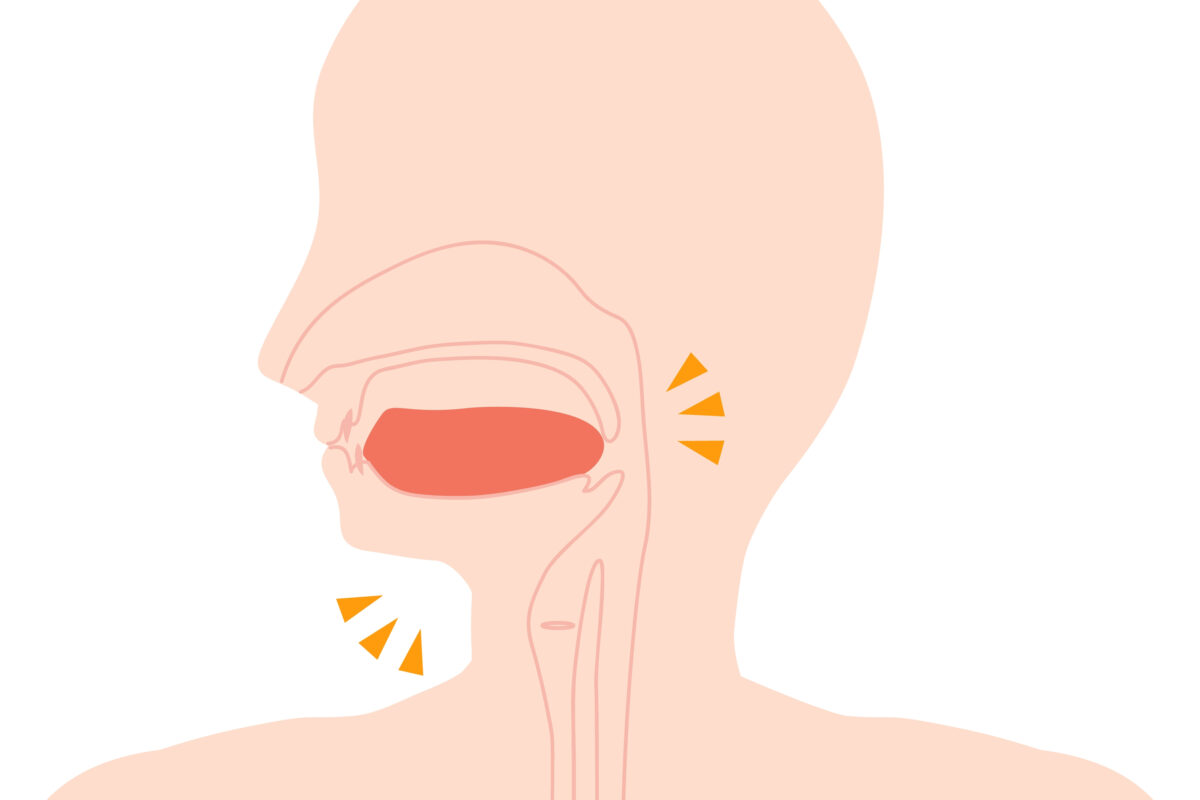
Screening comes first. Dentists or doctors might pull out the STOP-BANG or ESS quiz to spot people at risk for sleep apnea. Small signs get a closer look during a dental check, like a big tongue or a crowded throat.
If something seems off, the dentist sends the patient to a sleep specialist for testing. If sleep apnea shows up in the results, the doctor writes a prescription for a special oral device, mostly if a CPAP isn’t working well.
The dentist will then “fit” you with a custom mouthpiece, but the story doesn’t end there. Dentists stay in touch with the doctor, sharing updates on how the patient feels and what tweaks they make to the device. Every part of this loop aims to keep patients from slipping off the radar.
“Understanding the scope of practice as defined by the American Academy of Dental Sleep Medicine (AADSM) is an important first step,” states Capture 3D Radiology. “Dentists can obtain the knowledge and resources to screen patients for OSA, however, the DIAGNOSIS is made by a physician through questionnaires, physical examination, and the results of a sleep study. Dentists may participate in the management of the condition through oral appliance therapy (OAT) as an alternative to continuous positive airway pressure (CPAP) units, both of which must first be prescribed by the physician.”
Modern Device Standards for Oral Appliances
Getting a handle on the “dream team” approach for your customized dental sleep device starts with the basics. The rules set by the American Academy of Dental Sleep Medicine and the American Academy of Sleep Medicine are strict, and devices must be made for each person and adjustable.
Cheap boil-and-bite guards from the store don’t make the cut. Doctors say these can even do more harm than good.
A real oral appliance has to be Food and Drug Administration (FDA)-cleared as a Class II medical device. That means safe materials and strong construction, so it stands up to teeth grinding night after night. Fixed guards just can’t match that.
Adjustability isn’t a bonus — it’s required. These devices must let doctors slowly tweak the jaw’s position. Moving the lower jaw even a millimeter can make all the difference for breathing at night. Providers don’t just hand out mouth guards. They fit a medical device shaped for you and fine-tuned for your airway.
Picking how to treat OSA can feel overwhelming. Some patients need more support, and others want simplicity for everyday routines. The choice often boils down to two main options: CPAP machines or custom-made oral devices.
Here’s a side-by-side look at both approaches:
| Custom Oral Appliance (OAT) | CPAP Machine Therapy | |
| Primary Mechanism | Mechanical jaw advancement | Pneumatic airway splinting |
| Portability | Fits in a pocket; no power needed | Requires carry-case and electricity |
| Maintenance | Brushing and ultrasonic cleaning | Daily reservoir and tube sterilization |
| Invasive Level | Minimally invasive; intra-oral only | Requires facial mask and tubing |
| Compliance Rate | Generally high (approx. 75-90%) | Generally lower (approximately 40-60%) |
| Titration Method | Manual 0.5mm mechanical steps | Automatic or manual pressure settings |
| Interdisciplinary | High (Requires MD and Dentist) | Moderate (Primary focus on MD) |
CPAP machine technology stands out since severe apnea keeps airways open, but Oral Appliance Therapy (OAT) gets picked more for mild to moderate cases. People are more likely to stick with a small mouthpiece than deal with a mask or hose at night.
OAT’s effectiveness leans on careful calibration by specialists, while CPAP’s results depend more on how people handle the sensation of steady airflow.
“For patients with mild to moderate sleep apnea, comfortable oral appliances may be a viable alternative to traditional CPAP therapy,” according to the State College of Dental Sleep Medicine. “Oral appliances shift the jaw forward during sleep, putting pressure on throat muscles to keep the airway open. These appliances are comfortable, effective, and portable, and for many patients, treatment with an oral appliance alone is enough to keep their airway open through the night.”
Pain, Problems, and Dental Sleep Device Solutions
Dental sleep device doctors team up with pain experts a lot these days. Your jaw sits close to your airway, so any movement to help you breathe better can affect those joints and nearby muscles.
A dental sleep exam goes way beyond just cleaning your teeth or checking for cavities. Dentists often use 3D scans like CBCT to look at your airway and jaw.
Dentists don’t rush this process. They press on muscles like your masseter and temples to spot any tight spots or pain.
Some patients come in with constant headaches or sore faces. For them, any dental device needs to avoid putting more stress on the joints. The dentist checks how far your jaw moves forward and side-to-side, because this helps them build a device that doesn’t push your jaw too far or mess with your ligaments.
These treatments can shift teeth slightly or change your bite in the morning, and patients learn simple tricks to get their bite back to normal. It can involve doing special jaw exercises or using a bite wafer when they wake up. That way, everything goes back to its usual place year after year.
Choosing an FDA-cleared device isn’t just about checking boxes. The shape of your jaw and how you move your mouth matter a lot. Someone grinding their teeth at night might need more flexibility side-to-side.
For them, one style works better than another, and some patients are also looking for a small, easy-to-pack device for trips. Others can’t stand bulky options that trigger their gag reflex.
Every patient has different needs, so getting the device to fit right is just the first step. Adjustment takes patience as dentists tweak the lower jaw in tiny steps — sometimes half a millimeter at a time. This slow process helps keep the jaw comfortable and lets your muscles get used to the change.
The dentist and your pain management doctor stop adjustments once you stop snoring or having apneas, but your joints still feel good. Finding that balance takes trial and error and careful listening to your body.
Questions, Answers, and More
Many patients have the following dental sleep device questions:
- Why can’t I just buy a snoring guard online? Online boil-and-bite guards lack FDA clearance for sleep apnea and are not titratable. More importantly, they are not fitted by a qualified professional who monitors your jaw health. Using an unmonitored device can lead to permanent bite changes, jaw joint damage, and, most dangerously, a false sense of security while your oxygen levels continue to drop during sleep.
- Will my insurance cover an oral appliance? Because OSA is a medical condition, OAT is typically covered under your medical insurance, not your dental insurance. A collaborative practice will work with your sleep physician to provide the necessary diagnostic codes and “letters of medical necessity” required for insurance reimbursement.
- Is the device uncomfortable to wear? Most patients describe a tight feeling for the first few nights, similar to a new orthodontic retainer. Because the calibration is done in small 0.5-millimeter increments, your muscles have time to adapt. If you experience sharp pain, your interdisciplinary team (specifically the pain management specialist or dentist) will adjust the design to protect your TMJ (Temporomandibular Joint).
- How long does a custom device last? With proper care, a high-quality, medical-grade oral appliance typically lasts between 3-5 years. Annual follow-up appointments are necessary to ensure the material remains integral and the fit remains precise.
- What if I already have a CPAP machine but can’t use it? This is a very common scenario. You should return to your sleep physician to discuss CPAP intolerance. They can then refer you to a qualified dentist for OAT. In some severe cases, a combination therapy is used, where a small oral appliance is worn alongside a CPAP at a lower pressure, making the air more tolerable.
- Will my teeth move? There is a small risk of minor tooth movement over several years. This is why the collaborative model is so important; your dentist will provide a morning repositioner to use for 10-15 minutes each morning. This exercise resets your jaw and teeth to their original alignment, significantly reducing the risk of long-term changes.
Dental Sleep Device Learning, Improvement, and Evidence
Oral sleeping treatment and dental sleep devices keep changing fast, which means keeping up means always learning more.
Instead of trusting hunches, every choice sticks to proven methods from trusted guidelines like AASM (American Academy of Sleep Medicine) and AADSM (American Academy of Dental Sleep Medicine). This means using clear sleep tests to check if devices still work well.
The team always looks to do things better since they use digital scans now for more comfort and accuracy than old putty molds. Sleep apnea lasts for years, so the care never really stops. Patients come back every year, and doctors and dentists check the device to make sure nothing broke.
Gums and teeth need checking too. If someone loses or gains weight or gets sick, plans might need a tweak.
When your doctors actually talk to one another, you benefit. Teamwork brings sleep apnea care up to the same level as other health problems. Collaboration between medical and dental experts often makes the difference.
Sleep shouldn’t be a rolling dice, so avoid chasing shortcuts. Find a group that gets how your throat, your jaw, and your daily life are all connected. Good outcomes happen when every specialist points their efforts toward your health.
Wellness and Pain
Find your dental sleep device by visiting Wellness and Pain. We offer conservative treatments, routine visits, and minimally invasive quick-recovery procedures. We can keep you free of problems by providing lifestyle education and home care advice.
This enables you to avoid and manage issues, quickly relieving your inhibiting lifestyle conditions when complications arise. We personalize patient care plans based on each patient’s condition and unique circumstances. Wellness and Pain can help improve wellness, increase mobility, relieve pain, and enhance your mental space and overall health.