Hearing directly from adults who live with sleep apnea as you treat sleep apnea can offer invaluable insights and advice. Their personal accounts highlight everyday realities: the hurdles faced, the successes celebrated, and the journey of adaptation.
Let’s take a look at some common experiences shared by patients using different treatments.
CPAP: A Masked Journey to Treat Sleep Apnea
Using a Continuous Positive Airway Pressure (CPAP) machine is a common solution among sleep doctors who study and treat sleep apnea. Patient experiences are wide-ranging, often shared through online forums, interviews, and studies.
Many users mention challenges. Mask discomfort is frequently cited, sometimes described with exasperation. Air leaks can cause irritation, often blowing air into your eyes.
It’s not uncommon to wake up having unknowingly removed the mask during the night. Also, dry mouth and a feeling of claustrophobia can be recurring issues. Some patients find the sensation of forced air difficult to tolerate.
There are other issues. The effect on partner intimacy in bed is also a sensitive, real concern for some couples. The practicalities of traveling with equipment can feel burdensome.
Some patients get frustrated if they don’t see results and feel energetic almost immediately. But this oftentimes will mean their mask or pressure just needs adjusting.
Despite the initial difficulties, many patients persevere and experience transformative benefits. Many report feeling completely changed, waking up refreshed with significantly more energy and mental clarity.
Whatever the outcomes, many recognize their device is important to their health. Spouses and partners often share in the relief, particularly from loud snoring.
Success can come down to persistence, finding the right mask and pressure settings, and working closely with health care providers. While challenging at first, many patients adapt over time, and some even develop a strong appreciation for how their device improves their lives.
Hypoglossal Nerve Stimulation is a Mask-Free Alternative
As a newer option to treat sleep apnea, positive patient feedback for Hypoglossal Nerve Stimulation is growing, often from those who struggled with CPAP.
Many users who found CPAP intolerable describe this innovation as a game changer, or at very least report that it works great. One major benefit is the freedom from wearing a mask and hose, which can improve quality of life and comfort in bed. For some, it resolves their sleep apnea entirely.
There are important factors to consider. Strict eligibility criteria means it’s not an option for everyone, and it requires surgery to implant the device. Sensations from the nerve stimulation factor is a common topic discussed online. While some patients adapt, others find these little shocks or vibrating sensations uncomfortable.
This is especially true for higher settings needed for more severe apnea. Tongue soreness can also develop.
It’s worth noting that the effectiveness of this treatment relative to CPAP can be a point of disagreement among users.
Oral Appliance Therapy to Treat Sleep Apnea
Oral appliances, worn in the mouth like a mouth guard, offer another path to treat sleep apnea, with its own set of patient experiences.
For many, particularly those with milder Obstructive Sleep Apnea (OSA) or significant snoring, Oral Appliance Therapy (OAT) provides effective relief, offering deep sleep for many patients. It’s often seen as a viable alternative for individuals who can’t tolerate CPAP.
Side effects can be significant. These may include jaw pain, difficulty closing your mouth completely, and even Temporomandibular Joint (TMJ) dysfunction, which can sometimes be severe and long-lasting. A noticeable change in your bite alignment is also possible.
Success with OAT depends on the patient’s unique oral anatomy. For example, it may be less effective with a severe overbite.
Overall, it requires careful, expert fitting by a qualified pain management specialist, sleep doctor, or dentist. Cost and insurance coverage can also pose challenges for some patients.
The Role and Benefits of Lifestyle Changes
While devices and procedures are important solutions to treat sleep apnea, patients often highlight the role of changing their lifestyle habits and relying on external support.
Weight loss is cited as a factor, allowing patients to discontinue CPAP therapy, or at least reduce their treatment needs.
“Weight loss can reduce excess tissue around the airway, minimizing obstruction,” according to Yahoo Life. “Avoiding alcohol and smoking also helps by preventing airway relaxation and reducing inflammation.”
Perhaps most profoundly, spouses and bed partners often play a role, frequently being the first to notice symptoms like snoring or breathing pauses, urging the patient to seek diagnosis. They can also provide encouragement, helping you stick with your treatment.
Patients usually acknowledge the difficulty in making and sustaining lifestyle changes like diet and exercise. This spotlights an important point: sleep apnea treatment is highly individualized. What works wonderfully for one person might be intolerable for another.
Ultimately, success hinges not just on the treatment modality itself, but also on managing side effects, having realistic expectations about the process, and receiving adequate support from health care providers and loved ones.
Treat Sleep Apnea by Overcoming Your Barriers
Sticking with your treatment to treat sleep apnea isn’t always easy. Given the challenges, having support systems in place is vital for long-term success and receiving the full benefits.
Persistence and a willingness to problem-solve with your pain management specialist or health care team are imperative. Common issues have straightforward solutions:
- Mask Issues: Don’t hesitate to try different styles, such as nasal pillows, nasal masks, full-face masks, as well as different sizes to find the most comfortable fit for your face’s shape and your body’s sleeping position. Adjust the strap tension, which shouldn’t be overly tight and can cause leaks or discomfort. Mask liners or barrier creams can help protect your skin from irritation.
- Dryness or Congestion: Adjusting the heated humidifier on your machine is often the first step, experimenting with different humidity levels. Saline nasal sprays can help with congestion. If you tend to breathe through your mouth, a full-face mask might be necessary, or a chin strap used with a nasal mask to keep your mouth closed.
- Claustrophobia: Try gradual desensitization, where you wear the mask for short periods during the day while you’re awake and relaxed. Lower-profile masks like nasal pillows cover less of your face and may feel less confining. Practicing relaxation techniques before putting on your mask can also help.
- Pressure Intolerance: Discussing pressure adjustments with your sleep physician is important. Many machines offer comfort features like expiratory pressure relief, which lowers the pressure slightly when you breathe out. For some, an auto-adjusting PAP (APAP) or a Bi-level PAP (BiPAP) machine, which use different pressures for inhaling and exhaling, might be more comfortable.
Education, Support, and Telemonitoring are Important
To appropriately treat sleep apnea, understanding why treatment is important can be a powerful motivator. Beyond basic information, behavioral support from clinicians can help. Techniques like motivational interviewing or cognitive behavioral strategies, along with dedicated troubleshooting support, have been shown to help patients stay committed.
Many modern PAP devices come equipped with wireless modems that can send usage data directly to your health care provider. This telemonitoring allows clinicians to remotely track how many hours you’re using your machine, your residual apnea-hypopnea index (AHI), and mask leak levels.
This remote oversight is beneficial because it allows your doctor to identify problems early on, such as poor mask fit indicated by high leaks. They can intervene proactively.
It’s also often a requirement from insurance companies to demonstrate that you are using the therapy consistently for continued insurance coverage.
The Power of Peer Support to Treat Sleep Apnea
Solutions to treat sleep apnea don’t happen in a vacuum. The psychosocial aspects are incredibly important.
- Partner and Family Involvement: Engaging your partner or close family members in the education process can foster understanding and create a supportive environment at home. Addressing any concerns your partner might have, such as noise from the machine or impacts on intimacy, is also a part of the adjustment process for both of you.
- Support Groups and Online Communities: Connecting with others who live with sleep apnea can provide invaluable support. Online forums and patient advocacy groups, such as the American Sleep Apnea Association’s A.W.A.K.E. network, offer platforms to share your experiences, swap practical tips for managing challenges, and ask questions. You’ll also receive emotional support from fellow patients who truly understand what you’re going through.
This sense of community can minimize feelings of isolation and empower you. When exploring online forums, it’s a good idea to evaluate how active and helpful the community is.
By combining troubleshooting, professional guidance, utilizing technology like telemonitoring, and leveraging the power of social and peer support, you can increase your chances of successfully managing sleep apnea. This improves your health and quality of life.
Challenges, Causes, and Solutions
The powerful influence of patient partners and your peer support network highlights how managing personal circumstances to treat sleep apnea extends beyond the clinic.
Addressing any patient’s social context, facilitating partner involvement, and encouraging connection with peer communities can be powerful adjuncts to traditional medical interventions. This can improve long-term adherence, adaptation, and quality of sleep.
Treatment approaches that focus solely on your device or your specific medical condition, without considering psychosocial factors, may be less likely to achieve sustained success. Here’s a visual breakdown:
| Challenge | Potential Causes | Suggested Solutions/Tips |
| Mask Leak | Poor fit; improper size; worn-out cushion; incorrect strap tension; facial hair. | Readjust straps (snug but not overtight); try different mask size/style; clean cushion daily; replace cushion/mask regularly; consider mask liners; trim facial hair; consult provider/DME. |
| Dry Nose / Mouth / Throat | Air leak (esp. mouth leak with nasal mask); insufficient humidification. | Use/adjust heated humidifier; check for mask leaks; try a chin strap (with nasal mask); consider switching to a full-face mask; use saline nasal spray; stay hydrated. |
| Nasal Congestion / Runny Nose | Air pressure irritation; underlying allergies; insufficient humidification. | Use heated humidifier; saline nasal spray; treat allergies (nasal steroids, antihistamines – consult doctor); ensure mask fit to minimize direct airflow irritation. |
| Claustrophobia / Anxiety | Feeling confined by mask; anxiety about therapy. | Gradual desensitization (wear mask while awake); try minimal contact masks (nasal pillows); practice relaxation techniques before bed; discuss anxiety with provider. |
| Pressure Intolerance | Difficulty exhaling against pressure; pressure feels too high. | Use ramp feature (starts at lower pressure); discuss expiratory pressure relief features (C-Flex, EPR) with provider; consider APAP or BiPAP if CPAP intolerance persists. |
| Skin Irritation / Pressure Sores | Mask pressure; friction; allergic reaction to mask material; unclean mask. | Ensure proper fit (not too tight); clean mask daily; use mask liners or padding (memory foam, cloth); try different mask material; apply barrier cream (consult provider); allow skin breaks if possible. |
| Noise (Machine or Leak) | Machine malfunction; air leak from mask or tubing connection; filter issue. | Check all connections for leaks; ensure mask seal; clean/replace filters regularly; place machine below bed level or on a mat to dampen sound; contact provider/DME if machine noise is excessive. |
| Difficulty Falling Asleep | Discomfort; anxiety; noise; pressure sensation. | Practice good sleep hygiene; use ramp feature; relaxation techniques; ensure comfortable setup; allow time for adjustment; discuss with provider if persistent. |
| Bloating / Gas (Aerophagia) | Swallowing air, often due to high pressure or mouth breathing. | Ensure proper mask fit/type to minimize mouth breathing; discuss pressure settings with provider (may need adjustment); try sleeping position changes; consider BiPAP. |
| Travel Inconvenience | Bulkiness of machine; need for power source; airport screening. | Use a travel-specific CPAP machine (smaller, lighter); check airline policies (often allowed as carry-on medical device); bring necessary adapters/battery packs; plan ahead for power access. |
How Mouth Guards Work to Treat Sleep Apnea
Mouth guards designed to treat sleep apnea work through repositioning your jaw or tongue, opening the airway. By creating more space in the throat, these removable oral appliances help prevent your upper airway from collapsing during sleep.
They are intended for use only while sleeping and are frequently recommended for patients with mild or moderate Obstructive Sleep Apnea. However, they may provide benefits for those with severe cases too.
“Around 80% of sleep apnea cases are undiagnosed, while the main treatment is inconsistent,” states Cedars Sinai. “Just 30% to 60% of patients prescribed a continuous positive airway pressure (CPAP) mask reliably follow the regimen. In an effort to improve rates of care, sleep doctors are expanding treatment options.”
There are two primary types of mouth guards used for sleep apnea: Mandibular Advancement Devices (MAD) and Tongue Retaining Devices (TRD). While some newer devices are emerging, less research is available on their effectiveness in treating OSA.
MADs Versus TRDs and PAPs
Mandibular Advancement Devices to treat sleep apnea, also known as mandibular advancement splints or mandibular repositioning devices, are plastic mouth guards that cover your upper and lower teeth. Mandibular refers to the lower jaw.
MADs work by gently moving the lower jaw forward by several millimeters, which opens your airway. These devices can be a single, more rigid piece that limits mouth movement, or a two-piece system with linked components allowing for greater flexibility.
A qualified sleep doctor or dentist will create a custom-fitted MAD using a digital scan or an impression and bite registration of your teeth. Customization allows for variations in size, material, tooth coverage, jaw movement, and lower jaw advancement, among other features.
Customized MADs are more effective, comfortable, and better fitting than over-the-counter boil-and-bite versions. It’s important to note that premade MADs heated and molded at home are not Food and Druge Administration (FDA)-cleared for treating sleep apnea.
One concern with over-the-counter MADs is the potential for individuals to purchase them without a confirmed sleep apnea diagnosis or medical supervision. It’s important to work with a physician when considering MAD therapy.
Tongue-Retaining Devices (TRDs) use suction to hold your tongue in a forward position, preventing it from obstructing the airway. TRDs may be an option for individuals who lack sufficient teeth to anchor a MAD or who cannot use a MAD for other reasons.
TRDs have not been as extensively studied like MADs, making their effectiveness less clear. That’s why they’re prescribed and used less frequently.
For individuals who find Positive Airway Pressure therapy uncomfortable or difficult to use, sleep apnea mouth guards offer several benefits. These characteristics can make mouth guards a more manageable treatment option for some individuals.
Effectiveness, or Not, of Mouth Guards
Mouth guards to treat sleep apnea, particularly MADs, demonstrate immense effectiveness. However, it’s to a lesser degree than CPAP machines for some patients with respect to minimizing breathing pauses and improving blood oxygen levels.
Nevertheless, studies suggest MADs perform comparably to CPAP in alleviating daytime sleepiness, reducing snoring, and lowering blood pressure. MAD use may also contribute to less depressive symptoms and an improvement in your quality of life.
For certain patients, MADs are much more comfortable compared to CPAP machines, which can improve suitability for long-term use. While less extensively researched than MADs, TRDs may also help decrease breathing pauses, improve blood oxygen saturation, and lessen daytime sleepiness.
Ultimately, the success of any OSA treatment hinges on consistent use. Research indicates that approximately half of individuals prescribed CPAP therapy do not use it regularly or discontinue it entirely. If oral appliances like mouth guards prove more tolerable, patients are more likely to experience the benefits of treatment.
“While sleep apnea mouth guards are simple to use and often effective, they should not be used in certain situations,” according to the American Sleep Apnea Association.
Are Mouth Pieces Suitable to Treat Sleep Apnea
Some cases require urgent therapy to treat sleep apnea, such as severe OSA or daytime sleepiness that impacts driving safety. Experts typically favor CPAP in these situations.
Finding the optimal fit and adjustment for an oral appliance, in contrast, can often take several weeks or even months. Furthermore, individuals with significantly low blood oxygen levels during sleep, defined as falling below 70 percent, may not experience sufficient improvement with an oral appliance alone. In these cases, a mouth guard might not be adequate to address your severity of oxygen desaturation.
Certain dental conditions also contraindicate the use of MADs. These include having an insufficient number of teeth to secure the device, experiencing disease or immobility of your jaw joint, major periodontal disease, or an active gum infection.
People wearing teeth realignment devices like braces or retainers are also not suitable candidates for MADs. Any planned dental work, such as fillings or crowns, must be completed before an oral appliance is fitted to make sure it’s a proper fit and it functions the right way.
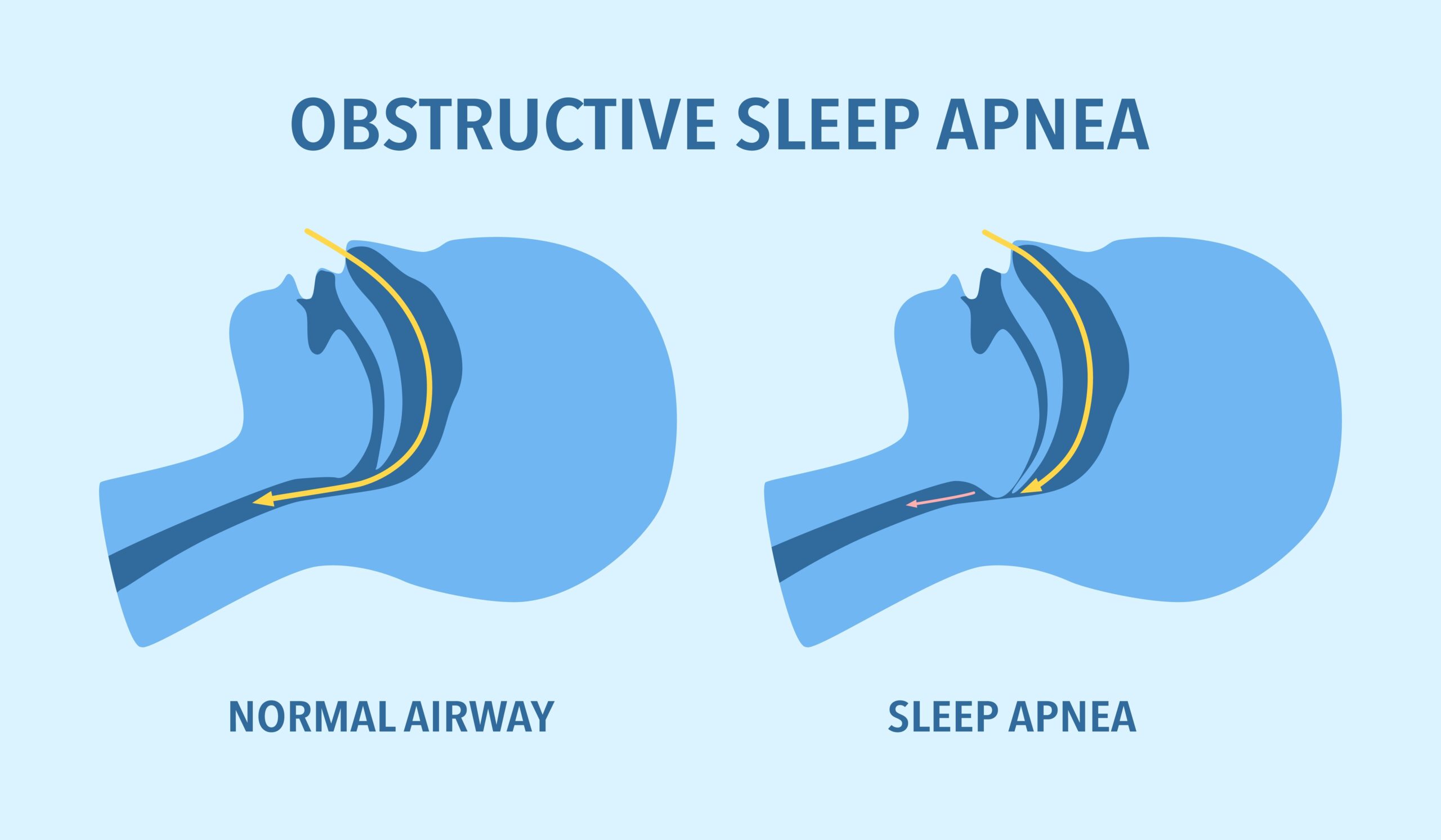
It’s important to distinguish between Obstructive Sleep Apnea and Central Sleep Apnea. While OSA is caused by a physical blockage of the airway, CSA results from your brain failing to send the proper signals to the body to breathe.
As mouth guards address the physical structure of the airway, they are ineffective for treating individuals diagnosed with Central Sleep Apnea. Consult your pain management specialist or sleep doctor for more information.
Wellness and Pain
Treat sleep apnea by visiting Wellness and Pain. We offer conservative treatments, routine visits, and minimally invasive quick-recovery procedures. We can keep you free of problems by providing lifestyle education and home care advice.
This enables you to avoid and manage issues, quickly relieving your inhibiting lifestyle conditions when complications arise. We personalize patient care plans based on each patient’s condition and unique circumstances. Wellness and Pain can help improve wellness, increase mobility, relieve pain, and enhance your mental space and overall health.