Immediate and Long-Term Relief for Your Calf Cramps at Night
Calf cramps at night can cause tight and knotted pain in your legs, and in some cases they last for several minutes. It may take days for your muscle to recover from a severe evening cramp without the right treatment.
Here’s a commonality: Leg cramps and Restless Leg Syndrome (RLS) both occur at night. In contrast to painful muscle cramps, RLS causes long-term discomfort and a physical desire to intermittently move your legs nearly all night long.
Nearly one in two people over the age of 60 suffer from a limited to chronic variation of nocturnal leg cramps, an issue that can impact your quality of life significantly. There is often a link between these cramps and other cramps elsewhere in the body, as well as high blood pressure, diabetes, venous insufficiency, and peripheral arterial disease (PAD).
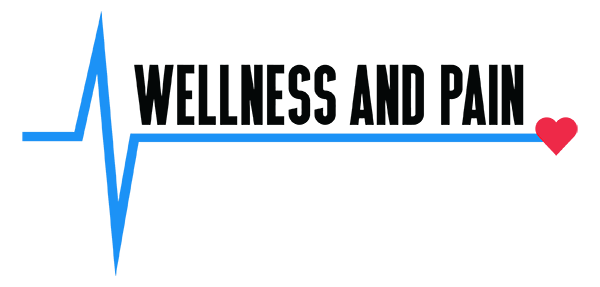
According to another study, 84 percent of patients with Chronic Venous Insufficiency (CVI) experience RLS or nighttime leg cramps. Untreated cramping, especially when your leg is swollen, can cause further complications. Some of these complications include discoloration or changes in skin texture, ultimately causing ulceration and infection.
To fully understand what’s going on when one or more muscles tighten suddenly and unexpectedly, it’s helpful to break down the science behind your chronic calf cramps into visuals and digestible nuggets.
Conditions and Factors Behind Your Calf Cramps at Night
The culprit behind your calf cramps at night can vary. They can happen from exercising or hard work — especially in the heat — and there are also some medicines and illnesses that cause bad muscle cramps.
Cramping occurs mostly in leg muscles, especially in the calf — usually lasting long enough to warrant anything from careful observation to actual treatment (or something in between). The area might be sore for hours or days after the cramp subsides.
Muscle cramps are usually harmless, but other incidents might come from medical conditions such as insufficient blood flow, nerve compression, or a mineral deficiency, leading to chronic calf cramps. When exercising, a cramping pain in your legs and feet can be caused by narrowing of your arteries that supply blood to the legs. As soon as you stop exercising, the cramps usually disappear.
Pressure on the nerves of the spine can also cause cramping pain in the legs. Walking usually worsens the pain in this situation. However, by walking slightly bent forward you actually ease the pain at times. This method looks and feels similar to when you push a heavy shopping cart.
Besides being overweight and not staying active, other factors can cause calf cramps at night:
- Sweating excessively. Playing sports often leads to muscle cramps for athletes who get tired and sweat a lot.
- Being pregnant. Extra weight and blood flow that accompanies the supply of oxygen and nutrients to a baby can cause muscle cramps.
- Your age. Age slowly decreases muscle mass. As a result, your muscles cannot work as hard as they used to. Sudden or harsh stimuli can stress them beyond what they’re capable of.
- Health and medical problems. Diabetes, liver disease, and thyroid illness can also cause muscle cramps. Other health or medical conditions impact them as well.
For the Time Being, Elevate Your Legs While Sleeping
Calf cramps at night can often be treated with a simple leg elevation pillow. These specialized pillows make sleeping more comfortable, ease lower back pain or knee pain, and assist in post-surgery recovery if needed.
But how does this work? Circulation is improved by raising your legs above your body. By raising your legs, your heart can more efficiently draw up oxygen-depleted blood from your veins. Whenever you raise your legs, you help deliver oxygen to every cell and every tissue in your body.
Leg elevation pillows can help ease inflammation, lower extremity swelling, and the pain inflicted by leg ulcers and varicose veins, as well as reduce the likelihood of blood clots. By flattening the lumbar spine, the pillows can also help decrease back pain. Overall, swelling and pain are reduced.
A leg elevation pillow usually has a washable cover, dense memory foam, breathable material, and a posture-boosting shape that makes it popular. You won’t feel like you’re lying on a board all night because it’s firm, yet soft. Non-slip pillows are designed with cooling gel foam to prevent overheating.
Sleep can feel elusive for those suffering from chronic calf cramps, but this “wedge” can make all the difference.
Besides using the pillow, you can stretch your calf and foot muscles before bed to prevent cramps. Also, moving around enough during every daily activity, errand, or chore can help, as well as drinking lots of water. When sleeping on your back, wear socks that are comfortable and supportive, and be sure your covers are loose.
Health, Lifestyle, and Prevention of Calf Cramps at Night
While neurological disorders, alcohol abuse, low blood sugar, hormone issues, insufficient vitamin intake, flat feet, pregnancy, and nerve damage are all related to calf cramps at night, a pain management specialist can identify the immediate steps you should take to improve your quality of life despite these conditions.
They include:
- Radiofrequency Ablation (RFA) or Endovenous Laser Ablation (EVLA). Fortunately, these are minimally invasive surgeries. Heat is delivered through a tube (catheter) to close the vein. Blood “pools” less once the vein is closed, and blood flow is improved.
- Sclerotherapy. This is for more serious cases. Specialists inject the affected veins with a unique chemical. As a result, the chemical scars the vein seals it off. In turn, blood redirects itself and finds healthier veins to flow through. As time progresses, your body actually absorbs the closed-off veins.
- Medications. A combination of compression therapy and medicines that increase blood flow through the vessels may help heal leg ulcers. In addition, after proper consultation with a doctor, you can also treat them with aspirin. However, doctors don’t usually recommend diuretics (medicines that pull excess fluid from the body through the kidneys). You can use them if other conditions such as heart failure or kidney disease also contribute to swelling. Diet can also cause chronic calf cramps. A lack of potassium, calcium, and magnesium can drastically affect your muscles. An eating lifestyle coupled with medications commonly prescribed for high blood pressure can cause these minerals to exit your body faster than they enter it.
- Surgical procedure. When the situation is severe, vein stripping is an option. Blood can no longer flow through the affected vein after the stripping, as veins with heavily damaged valves are removed.
Relief Starts with Diagnosis and Ends with Proper Treatment
First and foremost, you should incorporate a heart-healthy diet into your 24-hour lifestyle to help rid yourself of calf cramps at night. You can maintain a healthy circulatory system by limiting red meat, processed meats, processed and added sugars, salt and high-sodium foods, highly processed foods, saturated fats, and trans fats. Instead, increase your intake of vegetables, fruits, whole grains, legumes, fish, poultry, eggs, dairy, and olive oil or grapeseed oil when cooking.
Remember that cramping and aching legs can be prevented by treating the underlying vessel disease (usually vessel insufficiency). The goal of pain management is to close off problematic vessels and treat vessel insufficiency with a variety of minimally invasive, effective procedures.
Most commonly, weak or damaged vessels cause your chronic calf cramps. These compromised vessels prevent your body from cleaning waste and byproducts from your blood. However, most patients don’t necessarily exhibit these physical symptoms. This quandary is even in conjunction with varicose and spider veins. It’s common for leg cramps to be the only symptom of vessel disease if any symptoms exist at all.
Sclerotherapy or vessel ablation are usually the best treatments for leg cramps. It’s difficult to live with chronic calf cramps, but fortunately there is a cure.
Wellness and Pain Can Help
A range of options for treating calf cramps at night are available at Wellness and Pain. We offer conservative treatments, routine visits, and minimally invasive quick-recovery procedures. We can keep you free of problems by providing lifestyle education and home care advice to help you avoid and manage issues, quickly relieving the inhibiting lifestyle conditions when complications arise.
At Wellness and Pain, we personalize patient care plans based on each patient’s condition and unique circumstances to relieve pain, improve mobility and mental space, and improve your overall health.